|
 |
- Search
| Clin Exp Reprod Med > Volume 41(3); 2014 > Article |
Abstract
This article reports a case of spontaneous ovarian hyperstimulation syndrome (OHSS) following a thawed embryo transfer cycle. OHSS, a potentially life-threatening condition, is an iatrogenic complication of controlled ovarian stimulation; therefore, it is very important to prevent and treat OHSS during treatment with ovulation-inducing agents. Despite our efforts to prevent OHSS, in this case, severe spontaneous OHSS occurred, which resulted in uncontrolled preterm labor and a preterm delivery and also persisted for 6 weeks after delivery. Freezing all embryos cannot entirely prevent the development of OHSS because OHSS can occur spontaneously. Although spontaneous OHSS remains a rare event, females with a history of OHSS may have an elevated risk for spontaneous OHSS. We suggest closely monitoring cases of pregnancy following thawed embryo transfer for early diagnosis of spontaneous OHSS and the use of conservative management.
Ovarian hyperstimulation syndrome (OHSS), a potentially life-threatening condition, is an iatrogenic complication of ovarian stimulation with exogenous gonadotropins. OHSS typically occurs during either the luteal phase or early pregnancy [1]. Although the prevalence of severe OHSS is low, with reported values ranging from 0.2% to 1.2%, the syndrome remains a serious problem for infertility specialists due to its potentially fatal outcome [2,3,4,5]. The clinical manifestations of OHSS are ovarian enlargement, ascites, oliguria, abdominal pain, electrolyte imbalance, hemoconcentration, and thrombosis in severe cases [6,7,8]. The pathogenesis of OHSS is currently unknown. The primary pathophysiological mechanism underlying the development of OHSS is hypothesized to be an acute imbalance in the renin-angiotensin system. Moreover, increased levels of cytokines (interleukins and tumor necrosis factor-α), endothelin-1, and vascular endothelial growth factor have also been implicated in OHSS [9,10,11]. Human chorionic gonadotropin (hCG), either exogenously administered or as a result of endogenous pregnancy-derived hCG stimulation, is believed to play a critical role in the development of severe OHSS [9]. Several strategies have been proposed to reduce the incidence of OHSS during controlled ovarian hyperstimulation, including cycle cancellation, coasting, and modification of the ovulation triggering agents by decreasing the dose of hCG or employing GnRH agonist triggering [12,13,14]. Garcia-Velasco [15] reported that agonist triggering combined with oocyte vitrification and embryo transfer in a subsequent natural cycle prevented OHSS in at-risk patients and resulted in excellent cycle outcomes. In high-risk patients, the embryo transfer should be cancelled prior to the transfer on the fifth day [16]. In the case of severe OHSS, freezing of all embryos could be a last-resort measure to prevent OHSS. OHSS, however, while uncommon, can occur in normal spontaneous pregnancies [17]. Therefore, freezing all embryos would not entirely prevent OHSS.
The present case report is of a female with spontaneous OHSS (sOHSS) during a twin pregnancy after a thawed embryo transfer cycle. Freezing of all embryos was conducted to prevent OHSS. The severe sOHSS in the present case was not resolved until 6 weeks after delivery. The Institutional Review Board of the CHA Medical Center approved this report.
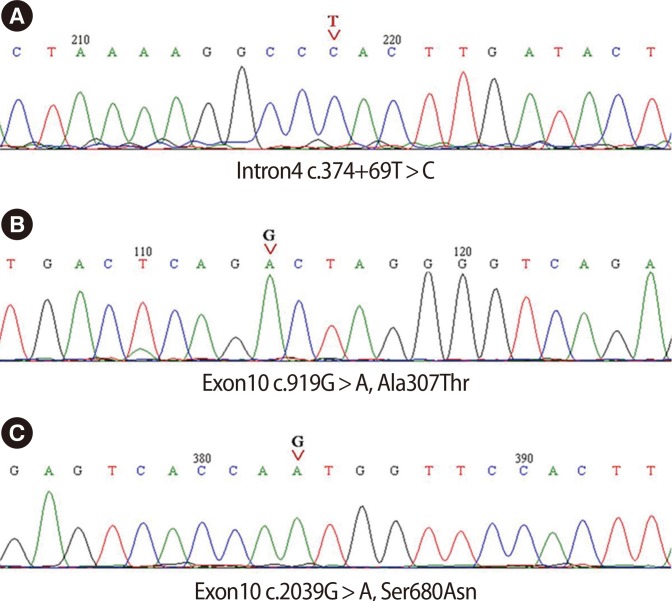
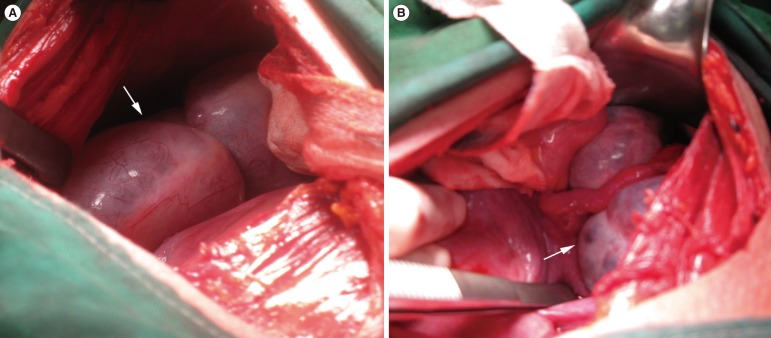
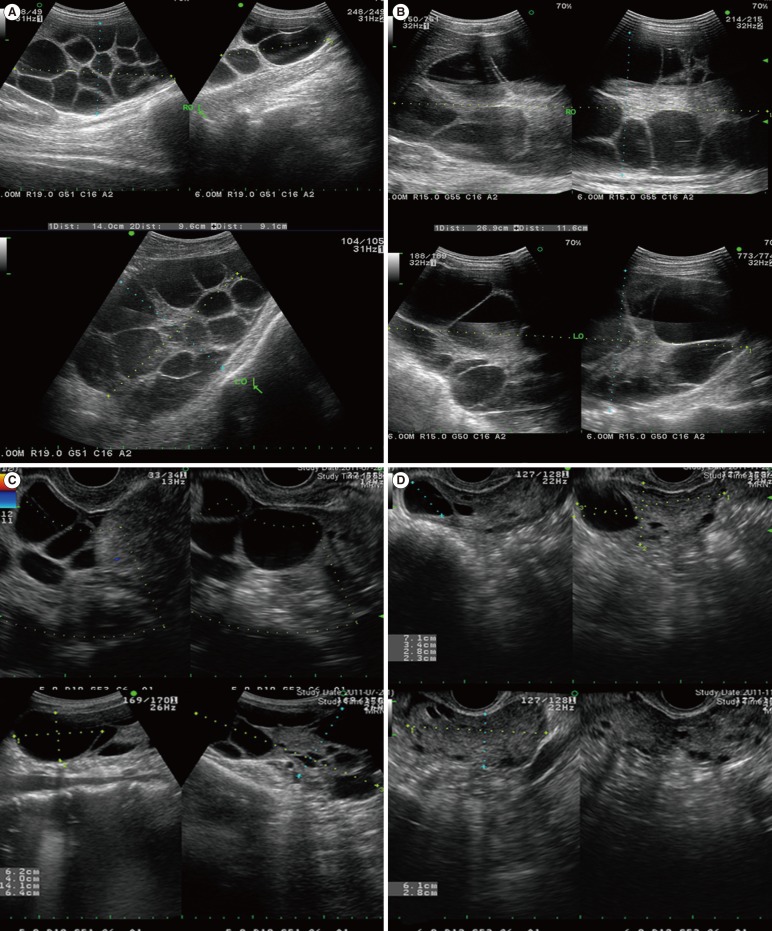
A 32-year-old nulligravida female presented with a two-year history of primary infertility. She had oligomenorrhea and features of hyperandrogenism. Polycystic ovaries were identified by transvaginal ultrasound and she was diagnosed with polycystic ovarian syndrome according to the 2003 Rotterdam consensus criteria. Her height was 155 cm, weight 44 kg, and body mass index (BMI) 18.31 kg/m2. No other history of illnesses or operations was noted. Following two cycles of ovulation induction and timed intercourse with clomiphene citrate and recombinant FSH, controlled ovarian hyperstimulation for assisted reproduction was performed using the GnRH antagonist protocol. Recombinant FSH (150 IU) was started on day three of the menstrual cycle and cetrorelix acetate (0.25 mg) was started on day seven. The FSH and E2 levels on day three were 5.4 mIU/mL and 29 pg/mL, respectively, and the total duration of stimulation was 9 days. 250 µg of recombinant human choriogonadotropin (r-hCG) was used to trigger ovulation; 27 follicles were aspirated and 25 oocytes were retrieved. Freezing of all embryos was performed because of high E2 levels (8,492 pg/mL) that were noted on day nine. In total, 18 oocytes were fertilized and cultured. Six out of 18 embryos developed to blastocysts and were vitrified using the previously described electron microscope grid method [18]. Three months later, following the identification of normalized ovaries, a hormonally manipulated artificial thawing embryo transfer cycle was conducted. Oral estradiol valerate (4 mg/day) was used (Progynova, Schering Korea, Seoul, Korea) beginning on day three of the cycle. On the fifteenth day of the cycle, the female's endometrial lining was 9 mm thick. Vaginal progesterone (600 mg/d; Utrogestan, Hanhwa Pharmaceuticals, Seoul, Korea) was prescribed. Warming of the embryos was performed using a previously described method [18]. Two embryos were transferred into the uterine cavity 5 days following the start of progesterone administration. Eleven days after the embryo transfer, serum β-hCG levels were >1,000 mIU/mL. A viable twin pregnancy was confirmed by transvaginal ultrasonography at 7 weeks gestation. During antenatal care, both ovaries abruptly became enlarged and cul-de-sac fluid was observed by transvaginal ultrasonography at 11 weeks gestation (Figure 1A). The patient was hospitalized with marked enlargement of the ovaries, ascites, and dyspnea, and a provisional diagnosis of OHSS was made. Her hematocrit was 35.5%, leukocyte 11,250/mL, and platelets 320,000/mL. Biochemical values were normal except for alanine transaminase (ALT), which was 55 IU/L. The FSH receptor (FSHR) gene was sequenced and one intron variation (c.374+69 C>T in intron 4) and two exon 10 variations (c.919 G>A Ala307Thr and c.2039 G>A Ser680Asn) were identified (Figure 2). The ovaries gradually enlarged to greater than 27 cm×12 cm and 26 cm×11 cm, respectively (Figure 1B). There were no symptoms of virilization. Cyst aspiration and paracentesis were performed at 13, 14, 16, and 20 weeks of gestation due to severe dyspnea from the massive ascites and large ovaries. At 21 weeks and 3 days gestation, preterm labor developed, but was controlled with Ritodrine (Lavopa JW Pharmaceuticals, Seoul, Korea). There were no other causes of preterm labor except increased abdominal pressure due to excessively enlarged ovaries and massive ascites. The fetuses appeared grossly normal on transabdominal and transvaginal ultrasonography, but the cervical length was shortened to <2.2 cm. At 22 weeks and 2 days gestation, membrane bulging developed and emergency cerclage was performed. The preterm uterine contractions were not controlled with Ritodrine (Lavopa, JW Pharmaceuticals, Seoul, Korea). The tocolytic agent nifedipin (niferon CR, Elysonpharm, Seoul, Korea) was given. The labor continued to progress, and atosiban was prescribed (tractocile, Ferring Korea, Limhamn, Sweden). In spite of these efforts to prevent a preterm delivery, labor continued to progress. A Caesarean section was performed at 26 weeks and 6 days gestation. Bilateral ovarian enlargement was noted (Figure 3). The pregnancy resulted in the live birth of a male weighing 1,050 g, and a female weighing 970 g. The Apgar scores of the male were 1 at 1 minute, 3 at 5 minutes, and 7 at 10 minutes and the Apgar scores of the female were 1 at 1 minute, 3 at 5 minutes, and 6 at 10 minutes. A postpartum follow-up ultrasound revealed that the hyperstimulated ovaries had improved, but they did not resolve until 6 weeks postpartum (Figure 1C). Normal ovaries were noted following transvaginal ultrasonography at 6 months postpartum (Figure 1D).
OHSS is an iatrogenic complication during the luteal phase or/and early stages of pregnancy following treatment with ovulation-inducing agents. Severe OHSS is considered a life-threatening condition and occurs in 0.2%-1.2% of stimulated cycles [2,3,4,5]. The incidence of OHSS continues to increase and fatal cases involving associated cerebral infarction, pulmonary thromboembolism, and massive pulmonary edema have been reported [6,7,8]. A recent report suggested that in the Netherlands maternal mortality rates from OHSS were three deaths per 100,000 IVF cycles [8]. Therefore, it is very important to prevent and treat OHSS during treatment with ovulation-inducing agents. According to the European Society of Human Reproduction and Embryology (ESHRE) guidelines, treatment with gonadotropins should be limited in patients at high risk for OHSS. Moreover, cycle cancellation, coasting, modification of the ovulation-triggering agent, administration of macromolecules, and cryopreservation of all embryos should be considered as secondary prevention [19]. Devroey et al. [20] recommended the concept of segmentation as a strategy to prevent OHSS. This strategy consists of optimizing ovarian stimulation, including GnRH agonist triggering in a GnRH antagonist cycle (Segment A), optimal cryopreservation methods for oocyte or embryo vitrification (Segment B), and embryo replacement in a receptive, non-stimulated endometrium in a natural cycle or artificial endometrial preparation (Segment C). Embryo vitrification, however, is not a definitive treatment. Although OHSS after spontaneous pregnancy is rare, it has been reported in pregnant women with hypothyroidism, in women with polycystic ovarian disease, molar pregnancies, pituitary adenomas, and in women with mutations in folliclestimulating hormone receptors [21,22,23,24,25,26]. The present report details a severe case of sOHSS that was not resolved until after delivery despite extensive efforts to prevent OHSS by using embryo vitrification and embryo transfer in a non-stimulated endometrium with artificial endometrial preparation. The case resulted in an extremely preterm delivery and hospitalization for over 3 months. Moreover, ovarian enlargement continued through the end of the pregnancy. Extremely enlarged ovaries may have been the cause of increased abdominal pressure and preterm labor. We attempted to decrease the ovarian size through reduction of the cyst by transvaginal ultrasound-guided aspiration, but the ovarian size increased again following aspiration. We investigated further to identify the cause of sOHSS, but only the Thr307/Asn680 (TN) allelic variant of the FSH receptor gene was present. The TN allelic variant has the highest frequency [27,28,29]. The genotypic variance of the FSH receptor has been described, including the impact of the FSH receptor genotypes at position 680 on ovarian responses to FSH stimulation. Patients with Asn in position 680 frequently respond well to exogenous FSH and are predisposed to respond quite intensely to exogenous gonadotropins. Theoretically, these individuals have a higher risk of developing iatrogenic OHSS [30]. Perez Mayorga et al. [31] showed that the FSH genotype in position 680 predicts severity in OHSS patients. Daelemans et al. [32] reported that an increased OHSS risk was noted in patients with the Ser680 allele in a study using a Caucasian control population. Interestingly, they found that among patients who developed iatrogenic OHSS, the more severe cases were women with the Asn680 variant. Therefore, the FSHR genotype in position 680 cannot predict the onset of OHSS, but rather may be a predictor of severity.
Of most interest in the present case, in addition to the occurrence of OHSS in a pregnancy following a thawed embryo transfer cycle, is that the onset of OHSS was not until 11 weeks of gestation and that the syndrome was still present several weeks after delivery. This case highlights the fact that although OHSS with a spontaneous pregnancy is rare, a twin pregnancy characterized by elevated β-hCG levels, bilaterally enlarged ovaries, ascites, and other physical findings suggestive of intravascular depletion may be the result of OHSS, and a corresponding diagnosis should be considered.
Females with a history of OHSS may have an elevated risk for sOHSS, but sOHSS remains a rare event. Nevertheless, a patient with a history of OHSS should be closely monitored. The present case demonstrates the importance of an early diagnosis and the role of observation and supportive care in the resolution of a potentially lethal syndrome. We suggest that single embryo transfer may decrease the probability of the development of severe OHSS in cases in which freezing of all embryos is used to prevent OHSS.
Notes
References
1. Delvigne A, Rozenberg S. Epidemiology and prevention of ovarian hyperstimulation syndrome (OHSS): a review. Hum Reprod Update 2002;8:559-577.PMID: 12498425.


2. Smitz J, Camus M, Devroey P, Erard P, Wisanto A, Van Steirteghem AC. Incidence of severe ovarian hyperstimulation syndrome after GnRH agonist/HMG superovulation for in-vitro fertilization. Hum Reprod 1990;5:933-937.PMID: 2150522.


3. Roest J, Mous HV, Zeilmaker GH, Verhoeff A. The incidence of major clinical complications in a Dutch transport IVF programme. Hum Reprod Update 1996;2:345-353.PMID: 9080231.


4. Abramov Y, Elchalal U, Schenker JG. Severe OHSS: An 'epidemic' of severe OHSS: a price we have to pay? Hum Reprod 1999;14:2181-2183.PMID: 10469676.


5. Andersen AN, Gianaroli L, Felberbaum R, de Mouzon J, Nygren KG, et al. European IVF-monitoring programme (EIM). Assisted reproductive technology in Europe, 2001. Results generated from European registers by ESHRE. Hum Reprod 2005;20:1158-1176.PMID: 15665021.


6. Cluroe AD, Synek BJ. A fatal case of ovarian hyperstimulation syndrome with cerebral infarction. Pathology 1995;27:344-346.PMID: 8771153.


7. Semba S, Moriya T, Youssef EM, Sasano H. An autopsy case of ovarian hyperstimulation syndrome with massive pulmonary edema and pleural effusion. Pathol Int 2000;50:549-552.PMID: 10886738.


8. Braat DD, Schutte JM, Bernardus RE, Mooij TM, van Leeuwen FE. Maternal death related to IVF in the Netherlands 1984-2008. Hum Reprod 2010;25:1782-1786.PMID: 20488805.


9. Delbaere A, Bergmann PJ, Gervy-Decoster C, Deschodt-Lanckman M, de Maertelaer V, Staroukine M, et al. Increased angiotensin II in ascites during severe ovarian hyperstimulation syndrome: role of early pregnancy and ovarian gonadotropin stimulation. Fertil Steril 1997;67:1038-1045.PMID: 9176441.


10. Levin ER, Rosen GF, Cassidenti DL, Yee B, Meldrum D, Wisot A, et al. Role of vascular endothelial cell growth factor in Ovarian Hyperstimulation Syndrome. J Clin Invest 1998;102:1978-1985.PMID: 9835623.



11. Elchalal U, Schenker JG. The pathophysiology of ovarian hyperstimulation syndrome--views and ideas. Hum Reprod 1997;12:1129-1137.PMID: 9221989.


12. Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Ross R, Morris S. Effects of the ovulatory serum concentration of human chorionic gonadotropin on the incidence of ovarian hyperstimulation syndrome and success rates for in vitro fertilization. Fertil Steril 2005;84:93-98.PMID: 16009163.


13. Garcia-Velasco JA, Zuniga A, Pacheco A, Gomez R, Simon C, Remohi J, et al. Coasting acts through downregulation of VEGF gene expression and protein secretion. Hum Reprod 2004;19:1530-1538.PMID: 15155606.


14. Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Ross R. Comparison of human chorionic gonadotropin and gonadotropin-releasing hormone agonist for final oocyte maturation in oocyte donor cycles. Fertil Steril 2007;88:237-239.PMID: 17296193.


15. Garcia-Velasco JA. Agonist trigger: what is the best approach? Agonist trigger with vitrification of oocytes or embryos. Fertil Steril 2012;97:527-528.PMID: 22222191.


16. Papanikolaou EG, Humaidan P, Polyzos N, Kalantaridou S, Kol S, Benadiva C, et al. New algorithm for OHSS prevention. Reprod Biol Endocrinol 2011;9:147PMID: 22054506.



17. Oztekin O, Soylu F, Tatli O. Spontaneous ovarian hyperstimulation syndrome in a normal singleton pregnancy. Taiwan J Obstet Gynecol 2006;45:272-275.PMID: 17175480.


18. Lee DR, Yang YH, Eum JH, Seo JS, Ko JJ, Chung HM, et al. Effect of using slush nitrogen (SN2) on development of microsurgically manipulated vitrified/warmed mouse embryos. Hum Reprod 2007;22:2509-2514.PMID: 17611188.


19. Delvigne A, De Sutter P, Dhont M, Gerris J, Olivennes F, Nygren KG. Ovarian hyperstimulation syndrome guidelines [Internet] 2013;cited 2014 Sep 20. Available from: http://www.gynera.ro/wp-content/uploads/2013/03/OHSS-LONG_GUIDELINES.pdf
20. Devroey P, Polyzos NP, Blockeel C. An OHSS-Free Clinic by segmentation of IVF treatment. Hum Reprod 2011;26:2593-2597.PMID: 21828116.


21. Leis D, Richter K, Schmid K. Spontaneous hyperstimulation of the ovaries with luteal cysts and ascites during a twin pregnancy-extreme case of the syndrome of painfull early pregnancy (author's transl). Geburtshilfe Frauenheilkd 1978;38:1085-1087.PMID: 569614.

22. Borna S, Nasery A. Spontaneous ovarian hyperstimulation in a pregnant woman with hypothyroidism. Fertil Steril 2007;88:705.e1-705.e3.PMID: 17433320.


23. Zalel Y, Orvieto R, Ben-Rafael Z, Homburg R, Fisher O, Insler V. Recurrent spontaneous ovarian hyperstimulation syndrome associated with polycystic ovary syndrome. Gynecol Endocrinol 1995;9:313-315.PMID: 8629460.


24. Ludwig M, Gembruch U, Bauer O, Diedrich K. Ovarian hyperstimulation syndrome (OHSS) in a spontaneous pregnancy with fetal and placental triploidy: information about the general pathophysiology of OHSS. Hum Reprod 1998;13:2082-2087.PMID: 9756273.


25. Baba T, Endo T, Kitajima Y, Kamiya H, Moriwaka O, Saito T. Spontaneous ovarian hyperstimulation syndrome and pituitary adenoma: incidental pregnancy triggers a catastrophic event. Fertil Steril 2009;92:390.e1-390.e3.PMID: 19356755.


26. Smits G, Olatunbosun O, Delbaere A, Pierson R, Vassart G, Costagliola S. Ovarian hyperstimulation syndrome due to a mutation in the follicle-stimulating hormone receptor. N Engl J Med 2003;349:760-766.PMID: 12930928.


27. Conway GS, Conway E, Walker C, Hoppner W, Gromoll J, Simoni M. Mutation screening and isoform prevalence of the follicle stimulating hormone receptor gene in women with premature ovarian failure, resistant ovary syndrome and polycystic ovary syndrome. Clin Endocrinol (Oxf) 1999;51:97-99.PMID: 10468971.


28. Simoni M, Gromoll J, Hoppner W, Kamischke A, Krafft T, Stahle D, et al. Mutational analysis of the follicle-stimulating hormone (FSH) receptor in normal and infertile men: identification and characterization of two discrete FSH receptor isoforms. J Clin Endocrinol Metab 1999;84:751-755.PMID: 10022448.


29. Sudo S, Kudo M, Wada S, Sato O, Hsueh AJ, Fujimoto S. Genetic and functional analyses of polymorphisms in the human FSH receptor gene. Mol Hum Reprod 2002;8:893-899.PMID: 12356937.


30. Loutradis D, Patsoula E, Minas V, Koussidis GA, Antsaklis A, Michalas S, et al. FSH receptor gene polymorphisms have a role for different ovarian response to stimulation in patients entering IVF/ICSI-ET programs. J Assist Reprod Genet 2006;23:177-184.PMID: 16758348.



31. Perez Mayorga M, Gromoll J, Behre HM, Gassner C, Nieschlag E, Simoni M. Ovarian response to follicle-stimulating hormone (FSH) stimulation depends on the FSH receptor genotype. J Clin Endocrinol Metab 2000;85:3365-3369.PMID: 10999835.



32. Daelemans C, Smits G, de Maertelaer V, Costagliola S, Englert Y, Vassart G, et al. Prediction of severity of symptoms in iatrogenic ovarian hyperstimulation syndrome by follicle-stimulating hormone receptor Ser680Asn polymorphism. J Clin Endocrinol Metab 2004;89:6310-6315.PMID: 15579795.


Figure 1
(A) Transvaginal ultrasonography indicated an enlarged left ovary with multiple follicular cysts at 11 weeks gestation, (B) gradually progressing enlargement of the left ovary at 13 weeks gestation, (C) slightly decreased size of the hyperstimulated ovaries at 6 weeks postpartum, and (D) resolution of the ovarian enlargement at 5 months after delivery. RO, right ovary; LO, left ovary.
-
METRICS

- Related articles in Clin Exp Reprod Med
-
Severe ovarian hyperstimulation syndrome in an oocyte donor despite preventive strategies ;0()
Prediction and Prevention of Ovarian Hyperstimulation Syndrome.2010 December;37(4)