|
 |
- Search
| Clin Exp Reprod Med > Volume 40(3); 2013 > Article |
Abstract
Objective
The majority of embryo transfers (ETs) to date have been performed on day 3 to reduce the potential risk of developmental arrest of in vitro cultured embryos before ET. Development of sequential media has significantly improved culture conditions and allowed blastocyst transfer on day 5. While day 5 ET provides higher clinical pregnancy outcomes with reduced risks of multiple pregnancies, it still has potential risks of developmental arrest of IVF embryos. The aim of this study was to evaluate the clinical outcomes of day 4 ETs and compare the efficacy of day 4 ET with day 5 ET.
Methods
From 2006 to 2009, a total of 747 fresh IVF-ET cycles were retrospectively analyzed (day 4, n=440 or and day 5, n=307). The cycles with any genetic factors were excluded. The rates of matured oocytes, fertilization, good embryos, and clinical pregnancy of the two groups were compared. The chi-square test and t-test were used for statistical analysis.
Results
There were no significant differences between the two groups with respect to the mean age of the females and rates of matured oocytes. The pregnancy outcomes of day 4 ET (40.7%) were similar to those of day 5 ET (44.6%). The implantation rate of day 5 ET (24.2%) was significantly higher than that of day 4 ET (18.4%) (p=0.003).
The pregnancy rate appears to be influenced by the culture environment used for the gametes. Many clinical researchers are concerned with suboptimal culture conditions for embryo development before embryo transfer (ET). Thus, some authors have recommended day 2 or day 3 ET to avoid expected suboptimal culture conditions due to the prolonged culture time [1-3]. However, the human embryonic genome is known to be activated at the 4 to 8 cell stage and early embryo quality evaluation based on embryo morphology on day 3 cannot accurately predict pregnancy potential [4]. Because of poor prediction of early cleavage stage embryo morphology, the number of transferred embryos needed for a successful pregnancy would be increased at day 3. However, an increased number of transferred embryos can increase the risk of multiple pregnancies [5,6]. Advances in culture media have enabled the change from early cleavage embryo transfer to blastocyst stage transfer in the practice of assisted reproductive technology (ART) [7]. Postponing ET to later stages can allow for better embryo selection and may significantly increase the implantation rate and reduce multiple pregnancies [8]. With the ability to select the most developmentally capable embryos, the number of transferred embryos can be decreased, thereby limiting high-order multiple pregnancies while maintaining an acceptable pregnancy rate [9]. However, day 5 ET at the blastocyst stage still has the potential risks of developmental arrest and reduced embryo quality in vitro, even with the most advanced sequential culture media [10].
In our center, day 4 ET cycles have been performed in preimplantation genetic diagnosis (PGD) cycles since 1995. We have reported successful pregnancy outcomes with day 4 ETs after PGD [11-14]. Based on the successful pregnancy outcomes in PGD cycles, we hypothesized that day 4 ET would have equivalent benefits of embryo selection for transfer to day 5 ET. Aiming for day 4 also has the advantage in a busy unit of enabling flexibility as to the day of embryo transfer between day 4 or 5 without affecting ongoing pregnancy rates.
From 2006 to 2009, a total of 747 fresh IVF-ET cycles were analyzed: 440 cycles on day 4 and 307 cycles on day 5 ET. The cycles with any genetic factors (PGD cycles) were excluded. The data collected included the age, infertility diagnosis, number of retrieved oocytes, matured oocyte rate, fertilization rate, and good embryo rate. The pregnancy outcomes were compared between day 4 and 5 ET.
Ovarian stimulation was performed using gonadotropin-releasing hormone agonist/antagonist, human menopausal gonadotropin, and human recombinant follicle stimulating hormone. Human chorionic gonadotropin (hCG) was administered when optimal follicle development was achieved, as evaluated by serial transvaginal ultrasound and estrogen determinations. Oocyte retrieval was performed via a transvaginal approach with sonographic guidance 34 hours after hCG injection. The IVF or ICSI was performed with the respective male partner's spermatozoa. Fertilization was assessed 16 to 18 hours after insemination by ICSI/IVF. The fertilized oocytes were cultured with G1.5 and G2.5 sequential media (Vitrolife, Kungsbacka, Sweden) until ET. After ET, if good grade embryos remained, they were cryopreserved for the next cycles.
The quality of embryos was graded using grading systems. Our grading system on day 4 was referenced from Tao's study [15] and grading of embryos on day 5 was referenced from Gardner's blastocyst grading system [16]. Briefly, the grade of I represented the best quality. Embryos of grade I, I-1, and II were considered to be 'good' embryos and grade II-1 and III were 'poor' quality embryos.
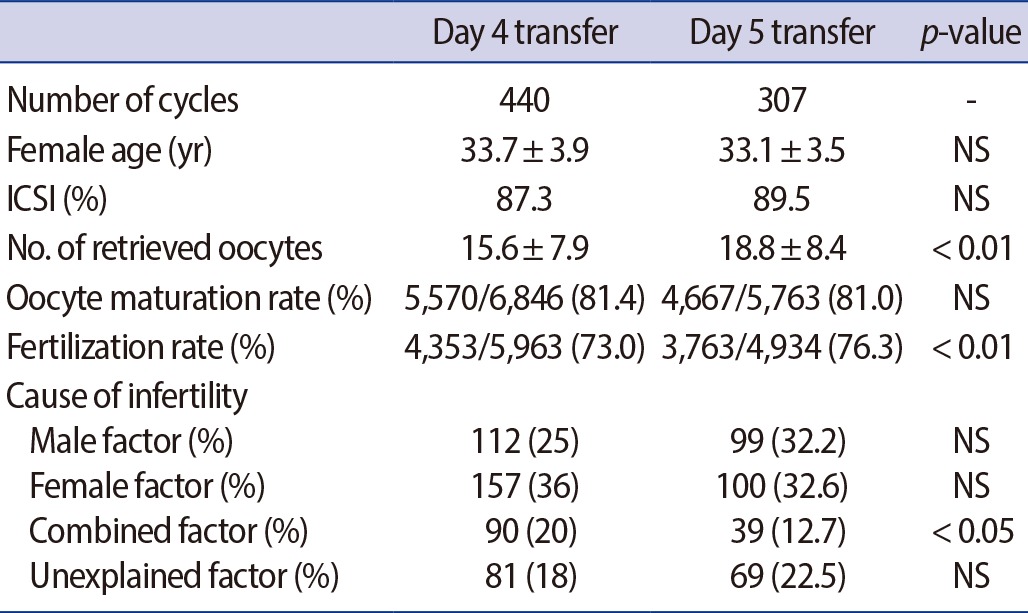
Cycle characteristics and fertilization outcomes are shown in Table 1. No significant difference was observed between the two groups regarding the female age and oocyte maturation rate. The fertilization rate and mean number of retrieved oocytes using day 5 ET were significantly higher than those using day 4 ET. The portion of male, female, and unexplained infertility factor were comparable between the two groups, except for combined infertility.
Of the embryos transferred on day 5, 85.9% were of good quality and 79.9% of the embryos transferred on day 4 were good. The proportion of good ET embryos was significantly different (p<0.01) between the two groups (Table 2). The mean number of embryos transferred on day 4 was significantly higher (p<0.01) than that on day 5. There was no significant difference in the clinical pregnancy rate between the two groups (40.7% vs. 44.0%), but the implantation rate of day 4 ET was significantly lower than that of day 5 ET (18.7% vs. 24.2%, p<0.05) (Table 3).
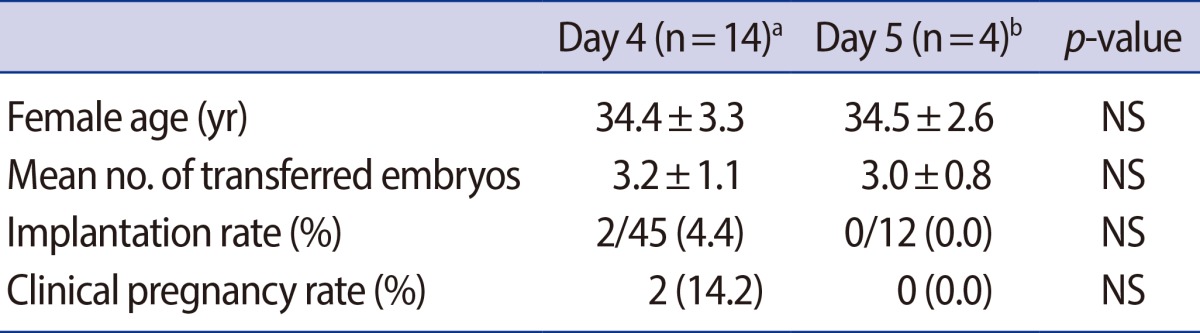
In the present study, we analyzed the pregnancy outcomes from slow developed embryos, which were defined as no embryos developed to morula and compaction on day 4 or no blastocyst formed on day 5. Interestingly, day 4 embryo transfer showed a 4.4% implantation rate and 14.2% clinical pregnancy rate even if there were no morula and compaction stage embryos. On the other hand, morula and compaction stage embryo transfer cycles at day 5 showed no implantation or clinical pregnancy (Table 4).
The selection of the most viable embryo for transfer is an increasingly important aspect of IVF-ET cycles. Advances in embryo culture media have allowed a longer period of embryo culture prior to transfer. Many studies have reported several advantages of blastocyst transfer. Blastocyst transfer improved embryo-uterine synchrony and allowed for a greater chance of selecting suitable embryos for transfer due to their having less chromosomal abnormality [17,18].
However, day 5 ET at the blastocyst stage still has potential risks of cycle cancelation due to developmental arrests and reduced embryo quality in vitro, even with the most advanced sequential culture media. Montag et al. [19] suggested that extended embryo culture is not beneficial when the option for embryo selection at later stages of development is not available.
The majority of ET in IVF-ET cycles is performed with early-cleavage stage embryos or blastocysts. It seems that the transfer of day 4 embryos has rarely been attempted by ART specialists even if such a transfer with embryos that have undergone compaction and reached the morula stage may have certain advantages [20].
Day 4 transfer is not disadvantageous for the following reasons: the embryo is returned to the uterus, to an environment where it would normally reside. The embryos can also be exposed to the uterine environment for the maximum time period and be in an in vitro environment for the minimal time period before implantation. In addition, uterine contractility is reduced at this time, all of which maximizes the potential for implantation [21].
The first report of pregnancy after transferring frozen-thawed morula/compact stage embryos was in 2001 from Tao et al. [15], and they noted a high survival and clinical pregnancy rate in frozen-thawed morula/compact stage embryo transfer cycles on day 4 [22]. In 2002, Tao et al. [15] published a retrospective study including day 4 and day 3 ET in which the authors proposed and followed a grading system for morula/compacted embryos; they reported that day 4 ET resulted in implantation rates similar to or higher than those of day 3 ET.
In our center, we have transferred morula stage embryos at day 4 in accordance with Tao's grading system. Cleavage stage embryos (e.g., 4- to 8-cell stage embryos) categorized as having slow development on day 4, were transferred in the absence of morula/compaction stage embryos. Slow developed embryos were transferred in fourteen cycles. Clinical pregnancies were achieved in two cycles (14.2%). In four cycles among the day 5 ET cases, in which all of the embryos had failed to form blastocysts, morula or compaction stage embryos were transferred. There was no clinical pregnancy in these cycles (0%) (Table 4).
In the present study, the implantation rate of day 4 ET was lower than that of day 5 (18.7% vs. 24.2%, p<0.05). However, the clinical pregnancy rates and multiple pregnancy rates of day 4 ET did not differ from those of day 5 ET (Table 3). Day 4 ET might allow for improvement of viable embryo selection compared with day 3 ET without the potential risks experienced in day 5 blastocyst transfer. Suboptimal culture conditions can originate from an excess number of IVF cycles, which may provide excessive loading for incubators due to excessive opening of the incubator door and increased time to reach an optimal pH and temperature [22]. To minimize excessive loading of culture systems and prolonged suboptimal culture conditions, day 4 ET can be chosen in a busy IVF unit. This strategy provides flexibility as to the day of ET, day 4 or 5, without affecting clinical pregnancy rates.
In conclusion, day 5 ET is well-known to be the best choice for an IVF-ET program. However, day 4 ET can be a useful option in a busy IVF laboratory because day 4 embryos still have a potential for implantation even if they have not reached the morula or compaction stages. Consequently, day 4 ET can be chosen to avoid ET cancellation in day 5 ET resulting from suboptimal circumstances in the IVF laboratory such as an excess number of IVF cycles beyond lab capacity or other suboptimal conditions for blastocyst culture. However, the decreased quality of embryos for transfer and the decreased pregnancy rate must be taken into consideration.
References
1. Quinn P, Stone BA, Marrs RP. Suboptimal laboratory conditions can affect pregnancy outcome after embryo transfer on day 1 or 2 after insemination in vitro. Fertil Steril 1990;53:168-170.PMID: 2295338.


2. Bolton VN, Wren ME, Parsons JH. Pregnancies after in vitro fertilization and transfer of human blastocysts. Fertil Steril 1991;55:830-832.PMID: 2010010.


3. Feil D, Henshaw RC, Lane M. Day 4 embryo selection is equal to Day 5 using a new embryo scoring system validated in single embryo transfers. Hum Reprod 2008;23:1505-1510.PMID: 18292597.


4. Braude P, Bolton V, Moore S. Human gene expression first occurs between the four- and eight-cell stages of preimplantation development. Nature 1988;332:459-461.PMID: 3352746.


5. Hershlag A, Floch JA, DeCherney AH, Lavy G. Comparison of singleton and multiple pregnancies in in vitro fertilization (IVF) and embryo transfer (ET). J In Vitro Fert Embryo Transf 1990;7:157-159.


6. Tan SL, Steer C, Royston P, Rizk P, Mason BA, Campbell S. Conception rates and in-vitro fertilisation. Lancet 1990;335:299PMID: 1967760.

7. Glujovsky D, Blake D, Farquhar C, Bardach A. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev 2012;7:CD002118PMID: 22786480.

8. Gardner DK, Schoolcraft WB, Wagley L, Schlenker T, Stevens J, Hesla J. A prospective randomized trial of blastocyst culture and transfer in in-vitro fertilization. Hum Reprod 1998;13:3434-3440.PMID: 9886530.


9. Skorupski JC, Stein DE, Acholonu U, Field H, Keltz M. Successful pregnancy rates achieved with day 4 embryo transfers. Fertil Steril 2007;87:788-791.PMID: 17224153.


10. Phillips SJ, Dean NL, Buckett WM, Tan SL. Consecutive transfer of day 3 embryos and of day 5-6 blastocysts increases overall pregnancy rates associated with blastocyst culture. J Assist Reprod Genet 2003;20:461-464.PMID: 14714825.



11. Lim CK, Cho JW, Kim JY, Kang IS, Shim SH, Jun JH. A healthy live birth after successful preimplantation genetic diagnosis for carriers of complex chromosome rearrangements. Fertil Steril 2008;90:1680-1684.PMID: 18076880.


12. Lim CK, Cho JW, Song IO, Kang IS, Yoon YD, Jun JH. Estimation of chromosomal imbalances in preimplantation embryos from preimplantation genetic diagnosis cycles of reciprocal translocations with or without acrocentric chromosomes. Fertil Steril 2008;90:2144-2151.PMID: 18440525.


13. Ko DS, Cho JW, Park SY, Kim JY, Koong MK, Song IO, et al. Clinical outcomes of preimplantation genetic diagnosis (PGD) and analysis of meiotic segregation modes in reciprocal translocation carriers. Am J Med Genet A 2010;152A:1428-1433.PMID: 20503317.


14. Lee HS, Kim MJ, Lim CK, Cho JW, Song IO, Kang IS. Multiple displacement amplification for preimplantation genetic diagnosis of fragile X syndrome. Genet Mol Res 2011;10:2851-2859.PMID: 22095609.


15. Tao J, Tamis R, Fink K, Williams B, Nelson-White T, Craig R. The neglected morula/compact stage embryo transfer. Hum Reprod 2002;17:1513-1518.PMID: 12042270.


16. Schoolcraft WB, Gardner DK, Lane M, Schlenker T, Hamilton F, Meldrum DR. Blastocyst culture and transfer: analysis of results and parameters affecting outcome in two in vitro fertilization programs. Fertil Steril 1999;72:604-609.PMID: 10521095.


17. Jones GM, Trounson AO, Gardner DK, Kausche A, Lolatgis N, Wood C. Evolution of a culture protocol for successful blastocyst development and pregnancy. Hum Reprod 1998;13:169-177.PMID: 9512252.


18. Milki AA, Hinckley MD, Fisch JD, Dasig D, Behr B. Comparison of blastocyst transfer with day 3 embryo transfer in similar patient populations. Fertil Steril 2000;73:126-129.PMID: 10632426.


19. Montag M, van der Ven K, Dorn C, van der Ven H. Extended embryo culture reduces the implantation rate on day 4 and day 5 when only a maximum of three embryos are cultured beyond the pronuclear stage. Eur J Obstet Gynecol Reprod Biol 2006;124:65-69.PMID: 16188376.


20. Pantos K, Makrakis E, Chronopoulou M, Biba M, Perdikaris A, Dafereras A. Day 4 versus day 3 embryo transfer: a prospective study of clinical outcomes. Fertil Steril 2008;89:573-577.PMID: 17517409.


21. Lesny P, Killick SR, Tetlow RL, Robinson J, Maguiness SD. Uterine junctional zone contractions during assisted reproduction cycles. Hum Reprod Update 1998;4:440-445.PMID: 9825859.


22. Zhang JQ, Li XL, Peng Y, Guo X, Heng BC, Tong GQ. Reduction in exposure of human embryos outside the incubator enhances embryo quality and blastulation rate. Reprod Biomed Online 2010;20:510-515.PMID: 20129824.