Effectiveness of emergency contraception in women after sexual assault
Article information
Abstract
Objective
To assess the effectiveness of emergency single-dose levonorgestrel contraception in preventing unintended pregnancies among woman who visited the emergency department (ED) due to sexual assault (SA).
Methods
We conducted a retrospective chart review in a university hospital in South Korea. Cases from November 10, 2006 to November 9, 2009 were enrolled. Information from the initial visit to the ED and subsequent follow-up visits to the gynecology outpatient clinic was collected.
Results
In total, 1,179 women visited the ED due to SA. Among them, 416 patients had a gynecological examination and 302 patients who received emergency contraception (EC) (1.5 mg single-dose levonorgestrel) at the ED due to SA were enrolled. Ten patients did not return for follow-up examinations. In follow-up visits at the outpatient clinic, two pregnancies were confirmed, which showed the failure rate of the EC to be 0.68%.
Conclusion
Single-dose levonorgestrel EC is extremely effective at preventing pregnancy among victims of SA.
Introduction
Sexual assault (SA) is a profound public health concern in South Korea, as it is around the world [1]. Based on the official statistics from the Supreme Prosecutors' Office of the Republic of Korea, between 1997 and 2006, the reported incidence of sexual assault increased from 15.1 per 100,000 to 27.7 per 100,000 of all women in South Korea, marking an increase of 83% in SA. The actual frequency of SA is assumed to be much higher, however. A 2007 survey using a representative national sample of 13,608 Korean college students revealed that the report rate for rape and attempted rape was estimated to be only 7.1% of the actual incidence [2].
The medical ramifications of SA may include acute and long-term physical and mental trauma, acquisition of sexually transmitted diseases, and unintended pregnancy. Unintended pregnancy may particularly result in significant social costs and individual risks, the greater part of which could be avoided by emergency contraception (EC) [3].
An unintended pregnancy resulting from SA poses tremendous mental and physical health trauma to the victim. One study revealed that pregnancy rates among SA patients vary between 1% and 5%, and half of these pregnancies end in an abortion [4]. This can lead to physical health problems, as well as a socioeconomic burden to the victim's community. EC provides a safe method of postcoital contraception that could reduce SA-related pregnancies by 88% to 95% if offered within a 120-hour window of the assault [5]. The first randomized trial to compare levonorgestrel (LNG) alone (two tablets of 0.75 mg taken at a 12-hour interval) with a combined oral contraceptive regimen (Yuzpe regimen) in EC was carried out in Hong Kong among women requesting emergency contraception within 48 hours of unprotected intercourse [6]. This study was important as the results suggested that the levonorgestrel regimen could mean an improvement to the Yuzpe method used for EC. They concluded that levonorgestrel was an effective drug for post-coital contraception with a lower incidence of side effects than the Yuzpe regimen. To confirm these findings, the Special Programme of Research, Development and Research Training in Human Reproduction (HRP) at the World Health Organization (WHO) planned a large randomized double-blind trial that started in 1995 [7]. The study produced three important findings: the levonorgestrel regimen of 0.75 mg twice with a 12-hour interval, was: 1) better tolerated; 2) more effective than the combined oral contraceptive regimen; and 3) with both treatments, the efficacy seemed to decline linearly with treatment delay [8]. The results of the trial had a tremendous effect on the interest among family planning providers and researchers in EC. Since publication of the results in 1998, the levonorgestrel regimen has been approved in 95 countries. Split levonorgestrel (0.75 mg given for two doses 12 hours apart) has been proven to be an effective regimen for an emergency. However, the dosing interval is inconvenient for those taking the first dose in the afternoon. According to the meta-analysis, a single dose of levonorgestrel (1.5 mg) administration seemed to have similar effectiveness to the standard 12-hour-apart split dose (0.75 mg twice) [9-11]. To date, this is the first study to examine the effectiveness of a single 1.5 mg levonorgestrel dose for EC among victims of SA.
Our hospital has been running a one-stop center for SA in the emergency department (ED) since 2006, to provide primary care for the victims of SA by a multidisciplinary team approach, and an important aspect of it is to prevent unintended pregnancies by providing EC. Accordingly, the aim of this study was to assess the effectiveness of emergency single-dose levonorgestrel contraception in preventing unintended pregnancy to patients visiting the ED due to SA.
Methods
This study was conducted in Ajou University Hospital, Suwon, Korea. The medical records for all women who received a single dose of 1.5 mg of levonorgestrel (Postinor, Bayer-Schering Korea, Seoul, Korea) for EC due to SA in the ED from November 10, 2006 to November 9, 2009 were obtained. Levonorgestrel (1.5 mg single dose) is the recommended therapy for EC at our institution. All patients were observed taking the medication by the provider. The EC had been offered up to 120 hours after sexual assault.
Complete medical records (electronic and hard copy) were reviewed by one of the study investigators to ensure that the patients included did receive the medication and that the data were recorded properly. Patients who were screened in the ED triage and did not obtain an examination for any reason were not included in this study. The institutional review board from our institution approved this study (AJIRB-MED-MDB-10-252).
Results
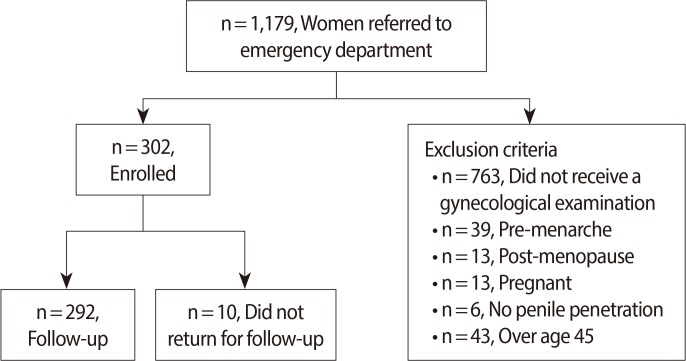
During a period of 6 months from November 10, 2006 to November 9, 2009, 1,179 women presented for evaluation after SA. All of the patients who had a gynecologic examination (416 women) and presented for a follow-up appointment at the outpatient clinic were enrolled. Among them, 71 did not receive EC for the following reasons: 39 patients were pre-menarche, 13 patients were post-menopausal, 13 patients were already pregnant, and 6 patients were not penetrated during the SA. The remaining 345 patients were prescribed EC. Among them, we excluded 43 patients who were over 45 years old. Therefore, there were 302 patients available for inclusion in this study (Figure 1).
Every patient who visited the ED due to SA had an initial urine pregnancy test administered. The mean age was 21.9±7.6 years old (from 12 to 44, 154 in their teens [51%], 112 in their twenties [37%], 30 in their thirties [10%], and 6 in their forties [2%]). Ten patients (3.3%) did not return for follow-up examinations to the outpatient clinic after the initial visit to the ED nor had sufficient interaction with our institution to confirm pregnancy. This population did not differ demographically and therefore had no effect on the sample. All of the patients received 1.5 mg of levonorgestrel as a single dose, and the majority of them received the medicine within 72 hours (294/302, 97.4%). Eight patients visited the ED 72 hours after the SA and received the EC between 72 hours to 120 hours after SA (8/302, 2.6%). No pregnancy was confirmed in these patients treated after more than 72 hours.
Prophylactic treatment for gonorrhea (ceftriaxone 125 mg intramuscularly), chlamydia (azithoromycin 1 g orally), trichomonas, and bacterial vaginosis (metronidazole 2 g orally) was given. If they wanted to know the results from the initial laboratory study or wanted medical certificates, or had any other complaints (e.g., vaginal discharge, pelvic discomfort etc.), they visited the same physician at the outpatient clinic within two weeks. After that, repeat serologic tests for syphilis, hepatitis B, and HIV were performed at 6, 12, and 24 weeks after the assault. A urine pregnancy test was performed again 3 to 6 weeks after the assault. Two patients whose pregnancy tests were negative at the primary visit to the ED had positive urine pregnancy test results during the follow-up visits (pregnancy rate, 0.66% [2/302]). One was in her late teens and the other in her early twenties. Thus excluding the 10 patients who did not return for follow-ups, the real pregnancy rate was 2 out of 292 (0.68%). Neither of the patients reported intercourse after the act of SA. Transvaginal ultrasonography was performed and an early intrauterine pregnancy was confirmed in both patients. They wanted a legal termination of the pregnancy, and we facilitated these requests. The police constabulary took genetic samples for the identification of the assailants after the terminations using conceptual tissue. The genetic samples taken matched further samples taken from suspects held in custody.
Discussion
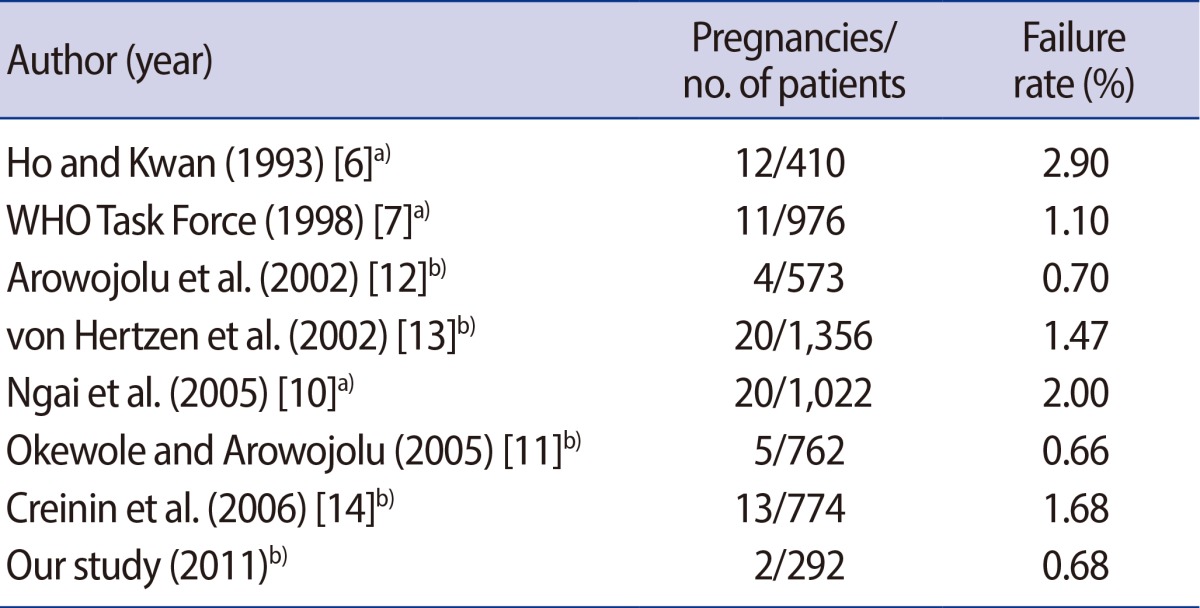
Our study shows that the emergency contraceptive, single dose levonorgestrel, is very effective for patients of sexual assault. The present study demonstrated a failure rate of 0.68%, which was less than or equal to previous reports on EC (Table 1) [6,7,10-14]. This confirms that 1.5 mg of levonorgestrel in a single dose is a highly effective method of EC in preventing unintended pregnancy for patients of SA.
Emergency contraception is using a drug or copper intrauterine device (Cu-IUD) to prevent pregnancy after unprotected sex. This is a back-up and not a regular contraceptive method. Mifepristone, ulipristal acetate, and levonorgestrel are very effective with few adverse effects, and are preferred to a combined estrogen and progestogen regimen. Levonorgestrel could be used in a single dose (1.5 mg) instead of two split doses (0.75 mg) 12 hours apart. The Cu-IUD is the most effective emergency contraceptive method and is the only emergency contraceptive method to provide ongoing contraception if left in situ [15].
A new oral tablet for EC, ulipristal acetate (UPA), is a selective progesterone receptor modulator and can be used up to 120 hours following unprotected intercourse, without an increase in adverse effects or a decrease in efficacy [14]. This selective progesterone receptor modulator is administered as a single 30 mg dose for EC. This agent provides a comparable, if not better, efficacy and side effect profile than that seen with levonorgestrel or mifepristone. Because it has both agonistic and antagonistic effects on the progesterone receptors, ongoing clinical trials are documenting UPA's use for patients with endometriosis and as an extended use contraceptive [16]. During the period of this study, we did not have UPA as an EC, so it was impossible to compare the efficacy of the two products. In the future, comparing UPA with single dose levonorgestrel as emergency contraceptives would be a valuable study.
Two trials have compared single-dose 1.5 mg levonorgestrel with two doses of 0.75 mg 12 hours apart. Arowojolu et al. [12] included 1,160 women who had a single act of unprotected intercourse within 72 hours of visiting the clinic, whereas von Hertzen et al. [13] included 4,136 women visiting within 120 hours of attending the clinic. There were no statistically or clinically significant differences between the two regimens in preventing pregnancy for all women (relative risk [RR], 0.77; 95% confidence interval [CI], 0.45-1.30). The key finding was that one dose of 1.5 mg levonorgestrel had efficacy equivalent with the divided two-dose regimen. In addition, the rate of side effects was very similar. Thus, there is no need to split the dose. In our study, over 97% of women were given EC within 72 hours of the act of SA, but 11 subjects received the EC after 72 hours. No pregnancy was reported in the latter cases. As we can see from these results, prescribing EC within 120 hours after SA should be recommended.
Low dose (<25 mg) mifepristone may be more effective than LNG (two doses of 0.75 mg each), but this finding was not conclusive. UPA may be more effective than LNG. LNG proved to be more effective than the Yuzpe regimen. The Cu-IUD was the most effective EC method and was the only EC method to provide ongoing contraception if left in situ [15].
A recent Cochrane review recommends that intermediate-dose mifepristone (25-50 mg) is superior to the LNG and Yuzpe regimens and should thus be the first choice for hormonal emergency contraception, and where mifepristone is not available, as in South Korea, a single 1.5 mg dose of levonorgestrel should be offered [9,15].
Our study has important limitations. It has no control group, is not a randomized prospective study, has small numbers, and some patients did not return for follow-up examinations. Naturally, EC must be provided for sexual assault patients, and therefore a control group is not possible among victims of sexual assault. Regarding the patients that did not return, if they were pregnant they should have visited our center because induced abortion for personal reasons is illegal in South Korea and SA victims need to prepare DNA evidence for a legal response to their assailants. Thus we presumed that in these cases there were no pregnancies.
There was particularly limited information on the last menstrual period or whether the patients had any sexual intercourse after the SA. Levonorgestrel EC is associated with significant but transient changes in menstrual patterns in a significant proportion of users [17]. They experienced intermenstrual bleeding and significant changes in menstrual cycle length, menstrual period length, and menstrual appearance compared to baseline patterns that differed according to whether EC was taken well before, close to, or well after the expected ovulation for that cycle. The majority of these changes disappeared in the following cycle. A study by Raymond et al. [18] found that, when taken in the first 3 weeks of the menstrual cycle, levonorgestrel EC significantly shortened that cycle as compared with both the usual cycle length and with the cycle duration in a comparison group of similar women who had not taken EC. Our study confirms (data not shown) that patients taking EC start menstruation earlier than expected. Some patients complained about intermenstrual bleeding within 7 days of receiving EC. Progestogen-only contraceptive methods (oral pills, implants, or progestin-only releasing intrauterine systems) are associated with frequent vaginal bleeding disturbances and breakthrough bleeding [19]. Although the pathogenesis of such breakthrough bleeding remains ill defined, it seems to be mediated via progestogen-induced down-regulation of sex steroid receptors and altered expression of local mediators that are implicated in menstruation [20,21]. Prospective research is needed on the effects of EC on victims of SA and the timing of treatment in relation to the menstrual cycle.
Our study demonstrates that a single 1.5 mg dose of levonorgestrel as EC after an act of SA is highly effective. Although this study has certain limitations, it confirms the recommendation that all patients seeking care after SA should be provided with an emergency single dose of levonorgestrel and encouraged to present for follow-up evaluation.
Notes
No potential conflict of interest relevant to this article was reported.