Effects of early prepubertal exposure to bisphenol A on the onset of puberty, ovarian weights, and estrous cycle in female mice
Article information
Abstract
Objective
Bisphenol A (BPA) is a chemical used extensively to manufacture plastics and epoxy resin liners for food and beverage cans. BPA, with properties similar to estrogen, has endocrine-disrupting effects. In the present study, we examined the effects of early prepubertal BPA exposure on the onset of puberty and reproductive parameters such as estrous cycle and reproductive organ weights in female mice.
Methods
Female mice were injected subcutaneously at postnatal day (PND) 8 with BPA (0.1, 1, 10, 100 mg/kg) in sesame oil or with sesame oil alone. Body weight was measured from PND 10 to 70. Vaginal opening and estrous cycle were monitored from PND 20 to 29. Animals were sacrificed at PND 25, 30, and 70, and the ovary and uterus weights were measured.
Results
Early prepubertal exposure to BPA (10 and 100 mg/kg) significantly decreased body weight from PND 18 to 30. BPA treated mice at testing dose levels showed early opening of the vagina compared to the control group. The number of estrous cycle and days of estrus were significantly decreased in high dose (100 mg/kg) BPA treated mice. The ovary weight at PND 25 and 30 was significantly decreased in all BPA treatment groups.
Conclusion
Early prepubertal exposure to BPA accelerated the onset of puberty but decreased reproductive parameters in female mice.
Introduction
Nowadays, humans are regularly exposed to numerous artificially synthesized chemicals, and concerns about the safety of these substances are on the rise. Recently, it has been reported that some of the synthetic chemicals worked as endocrine disruptors (EDs), affecting the reproductive endocrine system [1]. Studies on the genotoxicities of EDs have been cause for great concern. In vertebrates, the reproductive functions are maintained by hormones derived from the hypothalamic-pituitary (HP) axis and steroids from the gonads, which are influenced by the HP axis send feedback signals to the HP axis. To date, many reports have focused on the effects of EDs on sexual maturity and reproductive function [2-6].
Puberty can be divided into two subdivisions, central and the peripheral puberty. Central puberty consists of the onset of GnRH and gonadotropin secretions as the HP axis matures, the gonads are stimulated, the HP axis stimulates gonadal secretion of sex steroid hormones, and the steroids send feedback to the HP axis. Peripheral puberty consists of processes other than the activation of the hypothalamic-pituitary-gonadal axis. In the female, it includes secondary sex characteristics such as the development of mammary glands, the vaginal opening, and uterine hypertrophy [7]. Though the onset of puberty is a genetically driven event [8], it can be changed by environmental factors [9], nutritional states, and metabolic status. Even peripheral puberty has been induced by exogenous estrogenic stimulation [10].
Various exogenous factors such as lead [11], phytoestrogens [12], polychlorinated biphenyls (PCBs) [13], and pesticides [14] have also been shown to affect the onset of puberty in the animal model. In women, it has been postulated that the onset of puberty and the delay of breast development are affected by environmental factors [15-19]. Since precocious puberty has been linked to breast cancer, insulin resistance, bone development, and cardiovascular diseases [20], whether sexual maturation and puberty occur earlier after exposure to EDs is especially important to the field of health sciences. The onset of puberty is strongly influenced by environmental factors and intense psychological stressors [20]. Reports on the relationship between the time of puberty onset and chemicals including polybrominated biphenyls, dichlorodiphenyl dichloroethene, dichlorodiphenyl trichloroethane, and PCBs, have variously reported that menarche, pubarche, and breast development are advanced [15,21-24], conversely, that the onset of puberty is delayed [25-29], or that there is no clear relationship between them [17,30,31]. There is much debate regarding the relationship between exposure to EDs and the onset of puberty.
Bisphenol A (BPA) is used as a raw material in most plastics, and are used in the manufacturing of many food and medication containers, making exposure to it in modern life [32]. BPA is globally manufactured, is used in large quantities, and a considerable amount of it has been detected in the environment. In terms of environmental health, it is considered to be among the most important chemicals that must be managed [33,34]. BPA has weak estrogenic activity and acts on estrogen receptors to induce various gene expressions as well as disturb cellular signaling pathways [35,36]. In humans, BPA has been detected in breast milk [37,38], blood, follicular fluid, and placental tissues [39,40], and it has been shown to affect sperm quality, damage sperm DNA [41], delay the development of breasts, and trigger precocious puberty [42]. BPA concentration has been found to be high in patients with polycystic ovarian syndrome [43]. In rodents, BPA has been shown to affect indices of reproductive functions such as abnormal maternal behavior, egg deformation, sperm count reduction, fertilization rates, ovary and uterus weights, the distance between the genital pore and the anus, the time of vaginal opening, the sex ratio, survival rates, the number of neonates, gestation time, and the onset of the estrous cycle [44-48]. The relationship between the exposure to BPA, the onset of puberty, and sexual maturation is largely unknown. The infantile period is regarded to be a period of great vulnerability to exposure to EDs. In mice, exposure to estrogen 10 days after birth has been shown to be very responsive to the endocrine regulatory program of the HP axis. It is possible that exposure to estrogenic EDs in this period, more so than at other times, causes the most serious endocrine disrupting effects [49].
In the present study, to investigate changes in reproductive functions caused by EDs, experiments were performed to determine changes in body, ovary, and uterus weights, the time of vaginal opening, and the onset of estrous cycle after exposure to BPA in female mice.
Methods
1. Animals
Female mice (ICR strain) received mouse pellets and water ad libitum in a temperature- (22±3℃) and humidity-controlled (30%) room with 12/12 hours (light/dark) at the College of Natural Sciences, Hanyang University (Seoul, Korea). Female mice (postnatal day [PND] 8) were divided into four experimental groups, each of which received one of the following solutions, injected subcutaneously at 10 AM: 0.1, 1, 10, and 100 mg/kg of BPA solution dissolved in 100 µL of sesame oil (S3547; Sigma-Aldrich, St. Louis, MO, USA). The fifth group, the controls, were injected with only 100 µL of sesame oil. The number of mice in each group was 15.
2. Measurement of body weight gain
The body weight of five mice from each group were measured to the nearest 0.1 g at 10 AM from PND 10 to PND 70. And any apparent toxic effects including mortality, morbidity, and signs of injury were recorded at least once daily.
3. Examination of puberty onset and estrous cycle
To determine the onset of puberty for nine days from PND 20, the vaginal opening of five mice in each groups was checked at 10 AM daily. The estrous cycle was examined daily and identified under a microscope (×100) using a vaginal smear flushed with physiological saline for nine days from vaginal opening. Vaginal epithelial cell stained using methylene blue. During the nine days of checking the estrous cycle, the number of estrous cycles and days of confirmed estrus were recorded.
4. Necropsy and tissue weight measurements
The weight of reproductive organs were measured before and after the onset of puberty at PND 28, at PND 25 and 30, and PND 70 at adult period. The weights of ovaries and uteri obtained from five mice were measured in each group at PND 25, 30, and 70, after the mice were sacrificed by cervical dislocation after CO2 anesthesia to the nearest 0.01 g. Ovarian weight was calculated by averaging the sum of two ovarian weights in each animal. The major organs were also inspected for abnormalities at that time.
5. Statistical analysis
Numerical values were expressed as the mean±SD. Statistical analysis was carried out by one-way analysis of variance followed by Tukey's test for multiple comparisons among means. A p-value less than 0.05 was considered statistically significant.
Results
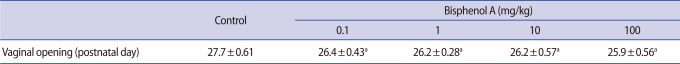
1. Changes of body weight by BPA in female mice
When compared to the control group, the 0.1 mg/kg and 1 mg/kg of BPA treatment groups showed no significant differences in body weight; however, in the 10 mg/kg of BPA treatment group, from PND 18 just prior to the time of puberty to PND 30 shortly after puberty, the body weight was significantly lower than that of controls. In the 100 mg/kg of BPA treatment group, the body weight was significantly reduced from PND 12 to PND 28. After PND 30, there were no significant changes in body weight between the treatment and control groups (Figure 1).
Changes in body weight after bisphenol A (BPA) treatment in female mice. Early prepubertal exposure to BPA (10 and 100 mg/kg) significantly decreased body weight from PND 18 to 30 (n=5 per group). aBPA 10 mg/kg, significantly different from control group at p<0.05; bBPA 100 mg/kg, significantly different from control group at p<0.05. Error bars are SD.
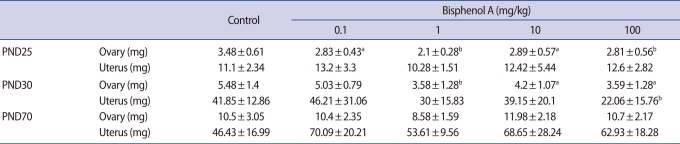
2. Changes in puberty onset according to vaginal opening
To determine the onset of puberty, the vaginal opening time was checked from PND 25 to PND 30. The first vaginal opening of the control group occurred on PND 26, and the first vaginal opening of all BPA treatment groups occurred on PND 25 (Figure 2). The mean days of the vaginal opening were identified as 27.7±0.61 in the control group, 26.4±0.43 in the 0.1 mg/kg BPA group, 26.2±0.28 in the 1 mg/kg BPA group, 26.2±0.57 in the 10 mg/kg BPA group, and 25.9±0.56 in the 100 mg/kg BPA group. The vaginal opening times of all BPA treatment groups were significantly faster than those of the control group (Table 1).
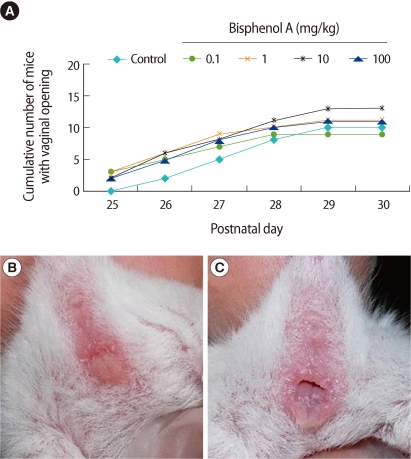
Effects of bisphenol A (BPA) on the onset of vaginal opening in female mice. (A) Vaginal opening of BPA treated mice at testing dose levels showed early opening of the vagina compared to the control group. (B) Photograph showing before vaginal opening and (C) after vaginal opening (n=5 per group).
3. Changes of estrous cycle after treatment with BPA
After treatment with BPA at PND 8, the number of estrous cycle was checked for nine days in female mice with a vaginal opening. It was slightly decreased in the 10 mg/kg and 100 mg/kg BPA treatment groups compared to the control group, but the differences were not significant. We checked the estrous cycle for nine days, and it was found that the number of estrous stages in the 0.1, 1, and 10 mg/kg BPA treatment groups was reduced when compared to the control, but the differences were not significant. However, in the 100 mg/kg BPA treatment group, the number was significantly smaller than the control (Figure 3).
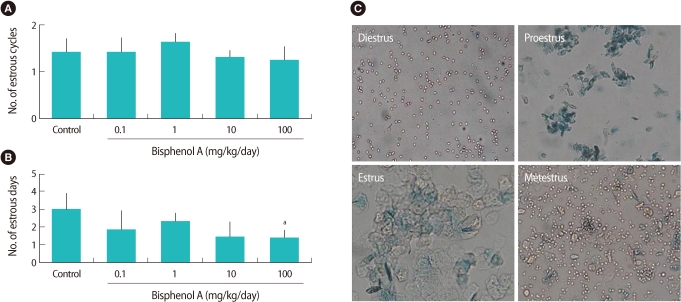
Changes in the estrous cycle after bisphenol A (BPA) treatment in female mice. (A) Change in the total number of estrous cycles during 9 days of vaginal smearing check. Changes in the total number of estrous cycles between the control group and the BPA treated groups were not statistically different. (B) Changes in the days of estrus during 9 days. Number of estrus days significantly decreased in the BPA 100 mg/kg treated group. (C) Smeared vaginal epithelial cells in each of the estrous stages (n=5 per group) (magnification×100). asignificantly different from control group at p<0.05. Error bars are SD.
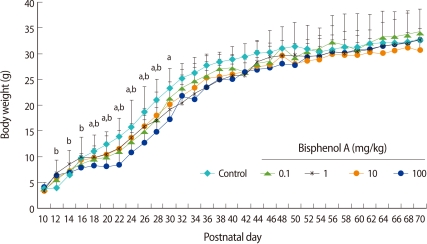
4. Changes of ovarian and uterine tissue weights after BPA treatment
At PND 25, the ovarian tissue weights of all BPA treatment groups were significantly lower than those of the control group, but the uterine weights were not. At PND 30, the ovarian weights in the 1, 10, and 100 mg/kg/day BPA treatment groups and the uterine weight in the 100 mg/kg/day of BPA treatment group were significantly lower than the control group. At PND 70, the adult stage, the ovarian and uterine weights in the BPA treatment groups were not significantly different from the control group (Table 2).
Discussion
A single administration of 10 mg/kg or 100 mg/kg BPA at PND 8 inhibited the increase of body weight from the lactiferous phase to just after puberty (PND 12 to PND 30). However, there was no influence on body weight at the adult stage (PND 35 to PND 70). Therefore, the amounts greater than 10 mg/kg BPA used in this experiment may have the capacity to inhibit growth to puberty. However, the systemic toxic effects of BPA in the adult stage are considered to be insignificant. At concentrations of 0.1 mg/kg or 1 mg/kg, BPA has no effects on body weight, and it was found that the vagina opened faster in the BPA treatment group than in the control group. Therefore, it can be postulated that the administration of estrogenic EDs to PND 8 lactiferous female mice did not induce any systemic effects, but changed peripheral puberty and consequently induced the early onset of puberty.
It has been reported that the mean concentration of BPA in human breast milk, blood, follicular fluid, and placental tissue is 0.6-2.4 ng/mL [39], and that the blood content of BPA is increased when one consumes canned fruit or drinks [50]. The safe intake limit of BPA allowed by the Korea Food and Drug Administration (KFDA) is 0.6 ppm, and it is equivalent to 0.01 mg/kg/day based on body weight of 60 kg. The lowest observed adverse effect level of BPA based on vaginal opening date identified in present study is 0.1 mg/kg and it is in excess of the safety limits defined by the KFDA. It is possible that reproductive transformation is more likely to happen when infants are exposed to BPA than adults because the susceptibility to reproductive transformation, such as the early onset of puberty by estrogenic substances, is high during the period of sexual differentiation of the brain in the infant stage [49], and since the female's hypothalamus is more susceptible to estrogenic stimulation than the male's. The incidence of early onset puberty is higher in women than in men [51]. In the present study, the early onset of puberty in PND 8 female mice was identified in the treatment group with a single administration of 0.1 mg/kg BPA, strongly suggesting that endocrine functions are likely to be disturbed by infantile exposure to BPA in humans.
Exposure to BPA in the infantile phase (PND 8) induced the significant reduction of ovarian weight in all BPA treatment groups at PND 25. In addition, ovarian weight at PND 30 was significantly reduced in 1, 10, and 100 mg/kg/day BPA treatment groups compared to the control group. However, at PND 70 there was no significant differences among the groups. It may be that the reduction of ovarian weight at PND 25 and PND 30 in the BPA treatment groups is due to the inhibition of follicular growth around puberty by infantile exposure to BPA. However, it is difficult to determine whether the reduction of ovarian weight at PND 30 is due to the impact of BPA or not, because the ovarian weight in the adult stage is different according to the ovarian follicular developmental stages.
BPA exposure during the infantile phase reduced the number of estrous stages and days. It is thought that this is due to the inappropriate development of the ovarian follicle associated with BPA exposure. It is considered that decrease in reproductive cycle reduced the ovulatory period in the fertile female and eventually induced the reduction of fertility. Similarly, it has been reported that estrogenic EDs such as BPA caused retardation of growth and reproductive functions, and this retardation of growth has a strong relationship to sexual maturity, the onset of puberty, oocyte quality, and fertilization capabilities in mice [4,52]. Infantile exposure to BPA did not induce changes in uterine weights at PNDs 25, 30, and 70. In the present study, infantile short-term exposure to BPA may not have altered uterine weight at adolescence and at the adult stage, because BPA was administered only once. On the other hand, it has been reported that cystic endometrial hyperplasia and adenomyosis in rats are induced in neonates for five days post partum after the pregnant mother receives 18 months of subcutaneous administration [53,54]. Therefore, the possibility that prolonged early lactational exposure to BPA may increase the various uterine lesions in senility cannot be ruled out.
In conclusion, it can be concluded that exposure to BPA during infancy increases the risk of precocious onset of peripheral puberty and the reduction of female reproductive fertility after puberty. Further studies are needed to study changes in central puberty regulated by the endocrine network in hypothalamic-pituitary-gonadal axis after exposure to estrogenic EDs, including BPA.
Notes
This study was funded by the grant from Korean Society of Pediatric Endocrinology 2009 and by the grant from Inje University School of Medicine 2010.
No potential conflict of interest relevant to this article was reported.