Factors influencing serum progesterone level on triggering day in stimulated in vitro fertilization cycles
Article information
Abstract
Objective
Elevated serum progesterone (P) levels on triggering day have been known to affect the pregnancy rate of in vitro fertilization (IVF). This study aimed to identify the possible factors influencing serum P levels on triggering day in stimulated IVF cycles.
Methods
Three hundred and thirty consecutive fresh IVF cycles were included in the study. All cycles were first attempts and were performed in a single infertility center. The indications for IVF were male factor infertility (n=114), ovulatory infertility (n=84), endometriosis (n=61), tubal infertility (n=59), unexplained infertility (n=41), and uterine factor infertility (n=39). A luteal long protocol of a gonadotropin-releasing hormone (GnRH) agonist (n=184) or a GnRH antagonist protocol (n=146) was used for pituitary suppression. Ovarian sensitivity was defined as the serum estradiol level on triggering day per 500 IU of administered gonadotropins (OS[a]) or the retrieved oocyte number per 500 IU of administered gonadotropins (OS[b]).
Results
Univariate analysis revealed that the serum P level on triggering day was associated with the serum estradiol level on triggering day (r=0.379, p<0.001), the number of follicles ≥14 mm (r=0.247, p<0.001), the number of retrieved oocytes (r=0.384, p<0.001), and ovarian sensitivity (OS[a]: r=0.245, p<0.001; OS[b]: r=0.170, p=0.002). The woman's age, body mass index, antral follicle count, and basal serum follicle stimulating hormone and estradiol levels were not associated with serum P level on triggering day. The serum P level on triggering day did not show significant variation depending on the type or cause of infertility, pituitary suppression protocol, or the type of gonadotropins used.
Conclusion
The serum P level on triggering day was closely related to the response to ovarian stimulation.
Introduction
Premature luteinizing hormone (LH) surges are a frequent cause of cycle cancellation in ovarian stimulation during in vitro fertilization (IVF) [12]. Even though the introduction of gonadotropin-releasing hormone (GnRH) analogues has dramatically decreased premature LH surges, there is still 5% to 30% chance of a subtle pre-ovulatory rise in the serum progesterone (P) during stimulated IVF cycles [34].
Controversy still exists about the association of clinical outcomes with elevated serum P levels at the time of ovulation triggering. Some have suggested that elevated serum P levels on triggering day are associated with negative clinical outcomes [14567], while others have reported no effect on clinical pregnancy rates [89]. Nonetheless, a recent meta-analysis comprising 63 eligible studies (55,199 fresh IVF cycles) found that P elevation on the day of triggering is associated with a decreased probability of pregnancy [10].
The mechanism through which elevated serum P levels on triggering day lead to a lower pregnancy rate remains unclear, but early P elevation may have an adverse effect on endometrial receptivity instead of affecting the quality of the oocyte or embryo [11]. Poor endometrial receptivity may be explained by premature endometrial maturation, which leads to embryo-endometrium dyssynchrony [12].
A subtle P elevation on triggering day might be a simple mass effect due to an excess number of follicles, which all produce a certain amount of P during ovarian stimulation [13]. Thus, it has been suggested that P elevation may reflect the response of mature granulosa cells to high exogenous exposure to follicle stimulating hormone (FSH) [10]. In fact, it has recently been demonstrated that high serum estradiol levels on triggering day are associated with a higher serum P level on triggering day [9]. Thus, P elevation is more likely to occur in high responders. In the present study, we identified patient characteristics and responses to ovarian stimulation that influence serum P levels on triggering day in stimulated IVF cycles.
Methods
1. Study population
This retrospective study included 330 fresh IVF cycles performed from October 2005 to October 2013 at the Seoul National University Hospital. In order to minimize bias, only the first cycle was included. Patients with polycystic ovary syndrome were excluded. This study was approved by the Institutional Review Board of the Seoul National University Hospital (IRB No. 1502-076-679). The indications for IVF were male factor infertility (n=114), ovulatory infertility (n=84), endometriosis (n=61), tubal infertility (n=59), unexplained infertility (n=41), and uterine factor infertility (n=39). The body mass index, basal serum level of FSH and estradiol, and antral follicle count were recorded if they were measured within two months before starting the cycle.
2. Stimulation protocols and IVF procedure
Controlled ovarian stimulation was performed using recombinant FSH (Gonal-F, Serono, Geneva, Switzerland) with or without highly purified human menopausal gonadotropin (Merional, IBSA, Lugano, Switzerland) or recombinant LH (Luveris, Serono) using the luteal long protocol of a GnRH agonist (Decapeptyl 0.1 mg/day; Ferring, Malmo, Sweden) (n=184) or the GnRH antagonist protocol (Cetrotide 0.25 mg/day; Serono) (n=146). When two or more leading follicles reached a mean diameter ≥18 mm, 250 µg of recombinant human chorionic gonadotropin (hCG) (Ovidrel, Serono) was injected. The oocytes were retrieved 36 hours after the hCG injection. Ovarian sensitivity was defined as the serum estradiol level on triggering day per 500 IU of gonadotropins (OS[a]) or the retrieved oocyte number per 500 IU of gonadotropins (OS[b]). The oocytes were inseminated by the conventional method (n=181) or by intracytoplasmic sperm injection (n=149), depending on the quality of the sperm and oocyte. The embryos were transferred three or five days after the retrieval of the oocyte. Luteal phase support was performed using either a daily dose of 50 mg of P in oil (Progest, Samil, Seoul, Korea) or 8% P gel (Crinone, Serono), starting on the day of oocyte retrieval. Pregnancy was first assessed 14 days after oocyte retrieval by analyzing the serum β-hCG levels. In cases with a positive β-hCG result, transvaginal ultrasonography was performed to confirm the intrauterine pregnancy and to identify the number of gestational sacs and the fetal heart rate. Clinical pregnancy was defined as the presence of one or more gestational sacs.
3. Statistical analysis
All statistical analyses were performed using the Statistical Package for Social Sciences software (PASW ver. 18, SPSS Inc., Chicago, IL, USA). The data were analyzed using the Kruskal-Wallis test or the Mann-Whitney test as indicated. The correlation test was performed by the parametric Pearson's test. Results were considered significant when the p-value was <0.05.
Results
The distribution of serum P levels on triggering day is depicted in Figure 1. The mean serum P level was 0.56 ng/mL (standard deviation, 0.45 ng/mL; range, 0.1-4.4 ng/mL). A serum P level on triggering day ≥1.5 ng/mL (considered an elevated serum P level according to the standard criteria) was observed in 4.2% of the population of the study (14/330).
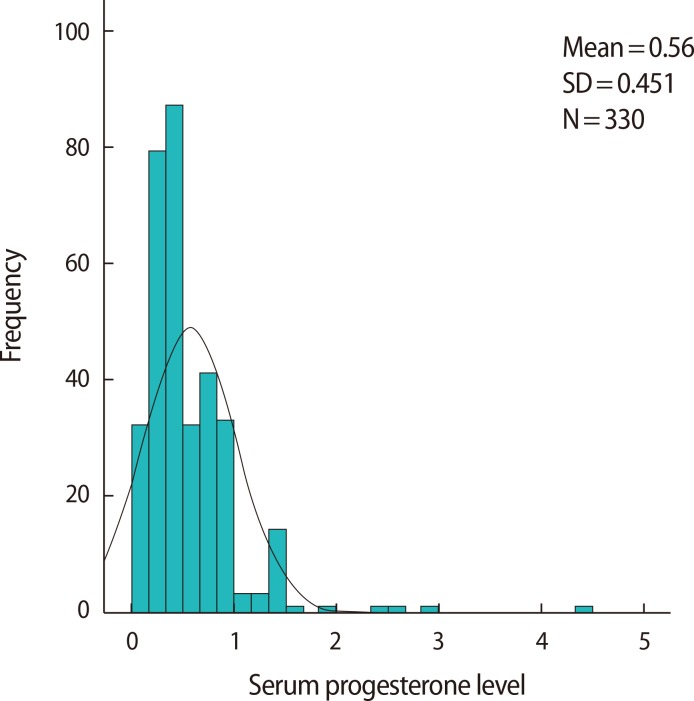
Histogram of serum progesterone levels on triggering day. The mean serum progesterone level was 0.56 ng/mL (standard deviation [SD], 0.45 ng/mL; range, 0.1-4.4 ng/mL).
Table 1 shows simple linear correlations between the serum P level on triggering day and various numerical parameters reflecting the outcomes of ovarian stimulation. The parametric Pearson's test revealed that the serum P level on triggering day was significantly associated with the number of follicles ≥14 mm (r=0.247, p<0.001), the serum estradiol level on triggering day (r=0.379, p<0.001), the number of retrieved oocytes (r=0.384, p<0.001), and both metrics of ovarian sensitivity (OS[a] r=0.245, p<0.001; OS[b] r=0.170, p=0.002). However, the woman's age, body mass index, basal antral follicle count, and basal serum FSH and estradiol levels were not associated with serum P levels on triggering day.

Linear correlations between serum progesterone level on triggering day and clinically relevant numerical parameters
Serum P levels on triggering day did not show significant differences depending on categorical parameters such as the type of infertility, the cause of infertility, the pituitary suppression protocol, and the type of gonadotropins (Table 2).
Among 330 IVF cycles, eight cycles were cancelled because transferrable embryos could not be obtained. Among 322 transfer cycles, clinical pregnancy was identified in 81 cycles (clinical pregnancy rate: 25.1%), and live birth took place in 73 cycles (live birth rate: 22.7%). The serum P levels on triggering day were similar between the groups in which pregnancy did and did not occur (0.57±0.37 ng/mL vs. 0.56±0.48 ng/mL). Dividing the study population into two groups according to the serum P level on triggering day likewise resulted in no significant difference in the clinical pregnancy rate (25.2% among patients with p<1.0 ng/mL vs. 23.1% among patients with p≥1.0 ng/mL).
Discussion
Our study demonstrated that serum P levels on triggering day were closely associated with the patient's response to ovarian stimulation. This finding is in agreement with a previous report, in which serum P elevation on triggering day was found to be closely related with a high estradiol level on triggering day, and thus was more frequent in high responders [9]. Another study has also shown that the serum estradiol level on triggering day and the number of oocytes were related to the occurrence of serum P elevation [10]. Gonadotropin dosage has been reported as a risk factor [1014]; however, we did not find a significant relationship between gonadotropin dosage and serum P levels on triggering day.
In the present study, serum P levels were found to be correlated with serum estradiol levels on triggering day and the number of oocytes, but not with gonadotropin dosage. With this in mind, we defined ovarian sensitivity as the serum estradiol level on triggering day per 500 IU of gonadotropins or the number of oocytes per 500 IU of gonadotropins. We demonstrated that ovarian sensitivity is closely associated with the serum P level on triggering day.
Several studies have demonstrated a correlation between reduced pregnancy and live birth rates and serum P elevation on triggering day [1456710]. However, few studies have attempted to assess the mechanism leading to elevated serum P levels after ovarian stimulation despite adequate pituitary suppression. In the present study, ovarian sensitivity was found to be a significant factor relating to serum P levels on triggering day. Thus, individual ovarian responsiveness should be considered when analyzing IVF outcomes according to serum P levels on triggering day.
In a recent study, the ratio of serum progesterone level to follicles (PFI) was shown to correlate more closely with IVF outcomes than serum P levels alone [15]. Thus, an elevated P level due to increased production per follicle (i.e., high PFI) would be detrimental, while an elevated P level due to additional follicular recruitment (low PFI) would not be detrimental. Thus, individual follicular production of P may be a factor that affects IVF outcomes in addition to serum P levels on triggering day.
In the present study, no difference was found in the serum P level on triggering day according to the method of pituitary suppression. Two previous reports have also confirmed these findings [116]. Moreover, no difference was found in the serum P level on triggering day between cycles with FSH alone and cycles with a combination of FSH and LH. According to the Menotrophin versus Recombinant FSH in vitro Fertilization Trial (MERiT) study, a higher incidence of serum P elevation was found in the FSH treatment group compared to the human menopausal gonadotropin treatment group (24.1% vs. 11.8%) [17]. In the FSH treatment group, there was no LH activity, which can convert P to androgen, and thus a higher level of serum P can be anticipated in cycles using FSH only. In our study, gonadotropins including LH were given in the late follicular phase, and therefore their P-lowering effect may be tenuous. This may explain why no difference was found in the serum P level between cycles with FSH alone and cycles with a combination of FSH and gonadotropins including LH.
The incidence of P elevation (≥1.5 ng/mL) was 4.2% in our study. This incidence was much lower than that reported in other studies [16]. In fact, previous studies show marked variation in the incidence of P elevation (4.2%-23%). Discrepancies in the characteristics of patients and/or treatment protocols may cause this variability.
In conclusion, our study provides new insights into the mechanism of serum P elevation on triggering day. Therefore, individual ovarian responsiveness should be kept in mind when interpreting elevated serum P levels on triggering day.
Notes
This work was supported by grant no. 800-2015-0065 from the Seoul National University College of Medicine Research Fund.
Conflict of interest: No potential conflict of interest relevant to this article was reported.
