A case of congenital cloacal exstrophy/omphalocele-exstrophy-imperforate anus-spinal defects syndrome and a successful pregnancy
Article information
Abstract
Herein, we report an exceptionally rare case of a 25-year-old woman with cloacal exstrophy/omphalocele-exstrophy-imperforate anus-spinal defects (OEIS) syndrome achieving a viable pregnancy despite many gastrointestinal and genitourinary malformations and multiple respective corrective operations. The patient was born with two vaginas, two uteruses, four ovaries, an imperforate anus, a large omphalocele including bowel and bladder exstrophy, and diaphysis of the pubic rami. This patient is the only documented OEIS patient not to have tethered spinal cord as an anomaly, perhaps contributing to her successful pregnancy. After experiencing preeclampsia with severe features at 35 weeks, the baby was born via cesarean section.
Introduction
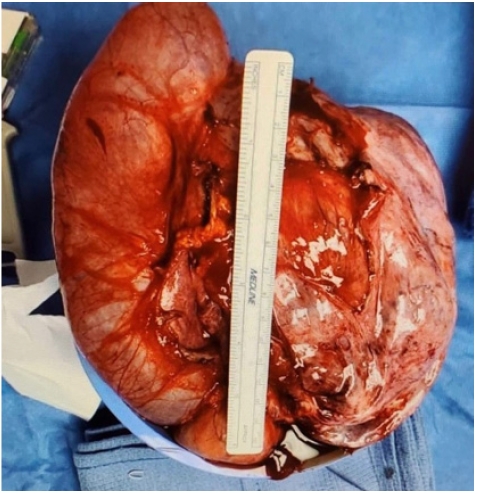
Cloacal exstrophy, a condition on the spectrum of omphalocele-exstrophy-imperforate anus-spinal defects (OEIS) syndrome, is regarded as being the most severe manifestation of exstrophy epispadias sequence (EES). While OEIS, exstrophy epispadias complex (EEC), EES, and cloacal exstrophy are often used interchangeably, the OEIS acronym specifically refers to omphalocele, exstrophy of the cloaca, imperforate anus, and spinal defects. OEIS is a very rare congenital defect resulting in an array of pathological phenotypes, with the most common being bladder and colon exstrophy, leading to a myriad of anomalies affecting multiple organ systems (Figure 1) [1,2]. Duplication of multiple sex organs is an additional phenotypic variant sometimes seen in OEIS patients. OEIS is estimated to affect 1 in 200,000 to 400,000 live births [1,3]. EEC refers to epispadias, classic bladder exstrophy, and cloacal exstrophy complex, with cloacal exstrophy being the most severe of the three abnormalities.
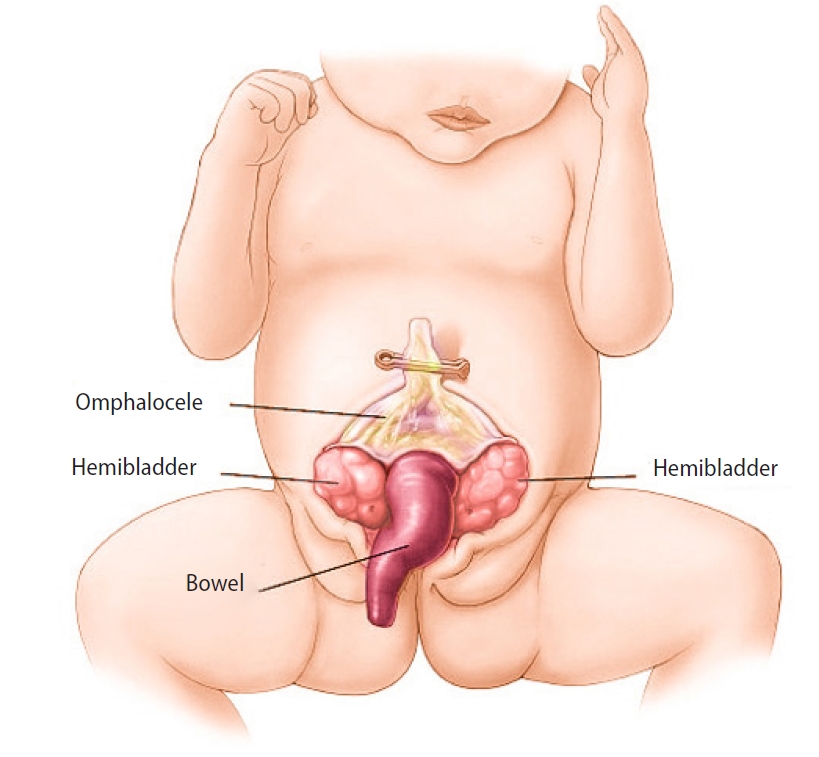
Demonstration of the typical cloacal exstrophy phenotype. The patient in this case study had those features in addition to didelphys uterus and two vaginas within the vulva. The image was recreated by Arielle Hough from Baby Excel's article on cloacal exstrophy (https://babyexcel.com/cloacal-exstrophy/).
Generally, early surgical intervention is preferred due to better outcomes relating to urinary continence, infection control, physical appearance, self-esteem, sexual function, and fertility [1]. Despite these better outcomes, most OEIS patients are rarely able to achieve a viable pregnancy because of their severe malformations. Their Müllerian anomalies lead to an increased risk of obstetric and urologic complications, but birth is possible. However, if they do achieve pregnancy, many risks are imposed [4]. The relatively fragile, reconstructed sexual organs typically cannot withstand the birthing process, and these patients also usually require additional postpartum operations [1]. These factors compel extensive obstetric and surgical evaluations throughout pregnancy, often warranting caution when an OEIS patient is considering conception. This paper presents the exceptionally rare case of a woman with OEIS syndrome who achieved viable childbirth and elaborates on various aspects of EES-OEIS, including prognosis and interventions. The Institutional Review Board approval was waived and informed consent was obtained from the patient.
Case report
A 25-year-old G1P0 woman born with OEIS syndrome presented to the office following a positive pregnancy test. Consistent with OEIS, this patient had many congenital malformations, including two vaginas, two uteruses, four ovaries, an imperforate anus, a large omphalocele including bowel and bladder exstrophy, and diaphysis of the pubic rami. This patient is the only documented OEIS patient not to have tethered spinal cord as an anomaly. The patient was given a colostomy bag until she turned 2 years old, when she underwent a colon pull-through procedure with continued regular enemas for bowel management. By age 4, she underwent a total hysterectomy and bilateral salpingo-oophorectomy, leaving her with a single uterus and cervix, bilateral fallopian tubes and two ovaries. Her second vagina with the vaginal cuff was closed off as well, leaving her with a single vaginal opening, which restored normal gynecologic anatomy. The patient had her bladder neck closed with a Mitrofanoff operation, as represented in the image below (Figure 2), urinating through a catheter through a stroma in the abdomen that she continues to use now. The patient began menstruating at 12 years old; she experienced irregular menstrual cycles on a sporadic basis, but was told this may happen. IRB waived and informed consent was given.
Despite her substantial surgical history, in June 2020, the patient learned she was pregnant after having several missed menstrual cycles. The patient had been counseled throughout most of her life by several specialists stating that her chances of pregnancy were substantially low. Because of this, the patient did not utilize any form of contraception. Once pregnant, additional extensive counseling took place regarding the high-risk nature of her pregnancy. Nonetheless, she decided to proceed with very close obstetric follow-up. The pregnancy was further complicated by a preexisting right-sided ovarian mass, the diagnostic impression of which was a benign ovarian cyst. The cyst was followed with serial sonography, which demonstrated progressive enlargement, quite possibly due to pregnancy-induced hormonal changes. At 35 weeks, the patient developed preeclampsia with proteinuria, necessitating delivery via primary cesarean section with ovarian cystectomy and/or possible salpingo-oophorectomy. Given her extensive adhesions from past corrective procedures and because of the large ovarian cyst requiring excision, cesarean section was performed via a midline vertical abdominal incision with a classical uterine incision [1,6].
At the time of delivery, the ovarian cyst measured approximately 30 cm (Figure 3). A viable male infant was delivered, weighing 1,842 g and measuring 41.91 cm. The hysterotomy was closed and attention was then turned to the right ovary. The mass had obliterated all normal ovarian architecture and a decision was made to proceed with unilateral salpingo-oophorectomy. The patient recovered well postoperatively and was discharged home on postoperative day 5. The pathology of the ovarian mass showed a benign ovarian cyst. The infant was admitted to the neonatal intensive care unit for 16 days and is reportedly doing well nearly 1 year after birth. The patient’s future fertility was preserved with a unilateral ovary and fallopian tube; however, the patient was extensively counseled on the high risk of complications for any future pregnancies. She was not placed on any birth control.
Discussion
A “typical” OEIS patient is difficult to define, as a spectrum of malformations can be found. The most common findings of OEIS, however, are omphalocele, imperforate anus, shortened hindgut, an open cecal plate flanked by open hemi-bladders on either side, and spinal cord and ureteral deformities [7]. Based on histopathologic studies in human embryos, current data attribute cloacal exstrophy to an early defect in the closure of the ventral body [8,9]. Cloacal exstrophy patients typically have normal ovaries (unlike our patient), but their Müllerian ducts do not fuse, resulting in uterine and vaginal duplication [7]. Some variants of OEIS result in the uterus remaining inside the body; however, patients often develop complications like uterine prolapse and intrauterine hemorrhage [9].
Few OEIS patients reproduce, limiting data on their offspring [1]. The current data do not demonstrate an association between cloacal exstrophy and aneuploidy, but also do not definitively exclude the possibility [8]. The exact underlying cause of cloacal exstrophy/OEIS is unknown and not currently attributed to any medications [10]. Many familial cases have been reported, suggesting an inherited component, but exact genetic relationships have not been found [11]. Interestingly, as with many other types of neural tube defects, it is highly associated with female monozygotic twins along with a risk of recurrence in subsequent pregnancies [8].
The OEIS complex comprises a wide spectrum of phenotypes, preventing a protocol-based standard of care. Each patient undergoes reconstructive operations pertaining to their own individualized malformations. Even after reconstruction, OEIS patients often experience life-long complications. As cloacal exstrophy is one of the most severe forms of an abdominal wall defect, always presenting with omphalocele, patients are frequently destined to suffer from bowel and urinary issues throughout their life [12,13]. One article studied the long-term functionality of patients born with OEIS syndrome and showed high rates of urinary and bowel incontinence in addition to constipation, with 42% of the patients requiring intermittent catheterization and 22% requiring urinary diversion [8]. Only 35% of female patients reported normal menstruation in this study [8]. Our patient reported that many doctors throughout her life stated that she would never get pregnant because of her malformations and history of multiple operations. The patient in this case report had cloacal exstrophy, as opposed to just bladder exstrophy, which is more commonly seen in anomalies with OEIS. A small study showed that out of 22 pregnancies in EEC patients, only 64% resulted in live births, none of which occurred in patients in the cloacal exstrophy group (i.e., live births only occurred in the bladder exstrophy patients) (Table 1) [14]. The glaring weakness of that study, however, is that it only had two cloacal exstrophy patients, an inevitable consequence of exceedingly rare conditions.
Only a few case reports exist of OEIS patients achieving pregnancy, substantially limiting the formulation of management guidelines [1]. Additionally, each case of OEIS syndrome varies greatly, further limiting standardization. The patient described herein is one of only a few in whom a live birth was reported. Fewer than 10% of women with cloacal and bladder exstrophy have been reported to have pregnancies, and these pregnancies were usually complicated by new-onset or worsening of recurrent urinary tract infections, uterine prolapse, and urinary incontinence [1].
In general, females born with OEIS can expect to face considerable challenges in life, not only relating to extensive operations and high-risk pregnancies, but also to urinary incontinence, poor body image, uterine prolapse, and fertility issues [6,13,15]. Documenting the rare success story of an OEIS pregnancy is vital for learning more about how to care for future similar cases. More data are not only needed regarding OEIS pregnancies, but also on the health and outcomes of the offspring. Additionally, further investigation is needed to elucidate some of the unique features of our patient that may have contributed to her successful pregnancy. Being the only known OEIS patient to not have a tethered cord could perhaps be one of those factors. Notwithstanding these patients’ many hurdles, pregnancy should not necessarily be ruled out early on in their life, as evidenced by the patient featured in this report.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Author contributions
Conceptualization: MS. Project administration: MS. Visualization: MS. Writing–original draft: MS. Writing–review & editing: MS, GG, MB, AH.