Natural conception rate following laparoscopic surgery in infertile women with endometriosis
Article information
Abstract
Objective
To investigate the influence of laparoscopic surgery on the natural conception rate in infertile women with endometriosis during the first year after the operation.
Methods
We retrospectively studied 43 infertile women with surgically proven endometriosis. The natural conception rate was investigated for the 12 months after the laparoscopy.
Results
The overall pregnancy rate was 41.9% (18/43). 66.7% (12/18) and 94.4% (17/18) of the patients conceived within postoperative 3 months and 6 months, respectively. The spontaneous pregnancy rate was not associated with the severity of endometriosis or laparoscopic findings or the type of surgery. The pregnancy rate for stage IV was relatively low (20.0%) compared to stage I, II, and III (35.7%, 44.4%, and 53.3%, respectively), although it did not reach statistical significance.
Conclusion
Conservative surgical treatment with laparoscopy and a prompt attempt at natural conception may be effective for infertile patients with endometriosis.
Introduction
Endometriosis is a common gynecological disorder that results in pelvic pain and infertility. The disease is known to affect approximately 10% to 15% of reproductive-aged women. When surgically investigated in infertile women, evidence of endometriosis was found in 30% of them, which rose to 50% if moderate-to-severe dysmenorrhea was present [1]. An association between infertility and endometriosis, albeit controversial, has been frequently reported. Although the mechanism by which endometriosis causes infertility remains unclear, several pathogenic mechanisms have been proposed, such as distorted anatomy in the pelvic cavity, a reduced quantity of functional ovarian tissue [2], and altered folliculogenesis [3].
The role of surgery in the attempt to improve the pregnancy rate in infertile women with endometriosis is much debated. Two randomized trials have compared laparoscopic surgical treatment of minimal and mild endometriosis with diagnostic laparoscopy only. Marcoux et al. [4] reported that laparoscopic surgery enhanced their fecundity but Gruppo Italiano [5] found no positive effect of surgery. The European Society of Human Reproduction and Embryology [6], the American Society for Reproductive Medicine (ASRM) [7], and the Royal College of Obstetricians and Gynaecologists [8] recommended surgery for stage I-II disease with limited benefit, and for stage III-IV disease with possible benefit.
In our previous study conducted from 1991 to 1998, the spontaneous conception rate during the 12 months after surgery was 48.5% and most of the conceptions took place during the first 3 months postoperatively [9]. As the number of subjects was small in the previous study, the present study was performed in a larger population in a longer period of 18 years.
Methods
The study subjects were recruited by review of medical records between 1991 and 2009, from infertile women who underwent operative laparoscopy at Seoul National University Hospital. The subjects from the previous study were also scrutinized and removed if ineligible. The eligibility criteria for recruitment were the following: age between 20 and 39 years; infertility (at least 12 months of unprotected intercourse in unsuccessful attempts to become pregnant); regular 24- to 35-day cycles; diagnosis of endometriosis based on surgical and histological criteria; no other infertility factors with confirmed bilateral tubal patency on hysterosalpingography; and no ovulatory drug therapy or assisted reproductive technologies (ART) or hormone therapy during postoperative 1 year. The review board for human research at the Seoul National University Hospital approved this project, and written informed consent was obtained from each woman. Laparoscopies were performed under general anesthesia. The stage of disease was determined by the revised American Fertility Society (rAFS) classification of the ASRM [10]. The laparoscopic surgical treatment involved the destruction or removal of all visible endometriotic implants and the lysis of adhesions.
The occurrence, during one year after the laparoscopy, of an intrauterine pregnancy was noted. The women's age, body mass index (BMI), duration of infertility, CA-125 level, primary or secondary infertility, stage of endometriosis, laparoscopic findings, and type of surgery were compared between the pregnant and non-pregnant group. All data analyses were performed using the SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Fisher's exact test and the Mann-Whitney U test were used as appropriate. The significance level for all analyses was a p-value of <0.05.
Results
One hundred fifty-four patients were diagnosed with endometriosis after a laparoscopic operation between 1991 and 2009. Twenty-seven patients were excluded for other infertility factors such as uterine synechiae, male factors, ovulatory disorder, and conversion to laparotomy. Forty-six patients received ART during the first postoperative year, 5 patients were under hormonal treatment such as GnRH agonist, and 33 patients were lost to follow up. Of the 154 women, 43 were eligible for assessment in this study and 18 patients (41.9%) successfully became pregnant during 1 year of natural ovulatory cycles.
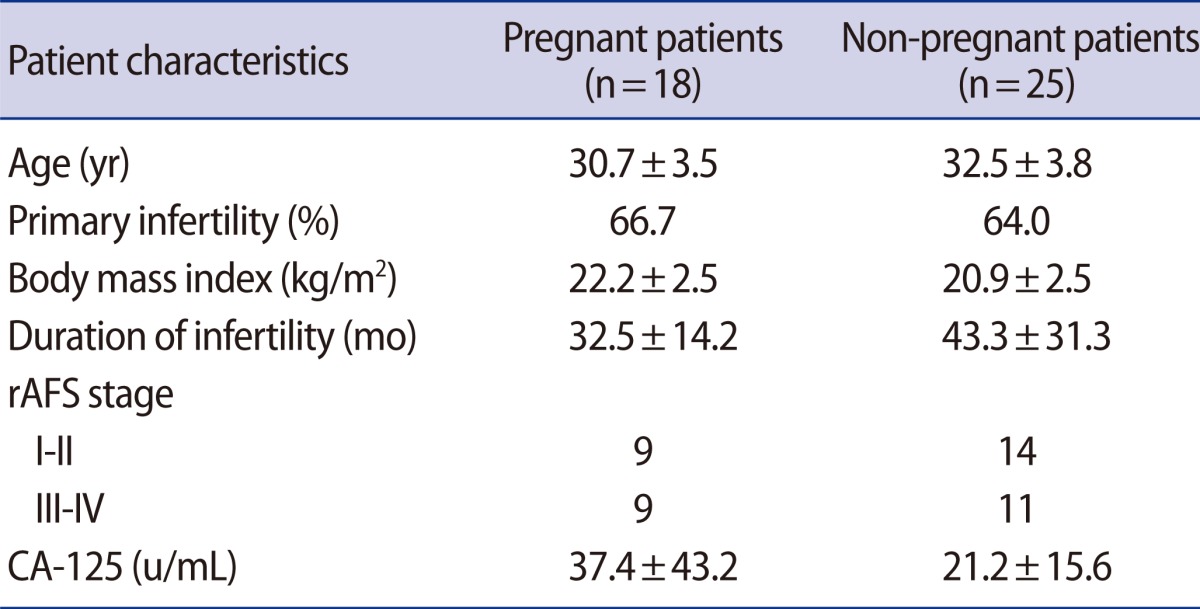
The patients' age, percentage of primary infertility, BMI, duration of infertility, rAFS stage, and CA-125 level were similar in the pregnant and non-pregnant groups (Table 1). The median duration of days from surgery to the last menstrual period was 60 days ranging from 1 to 270 days. 66.7% (12/18) and 94.4% (17/18) of the patients were conceived within postoperative 3 months and 6 months, respectively (Figure 1).
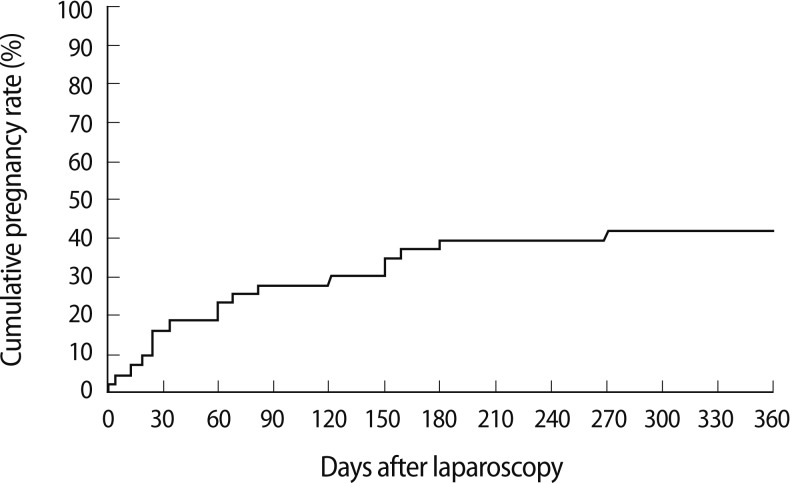
Cumulative intrauterine pregnancy rate in the 12 months after laparoscopy in women with endometriosis.
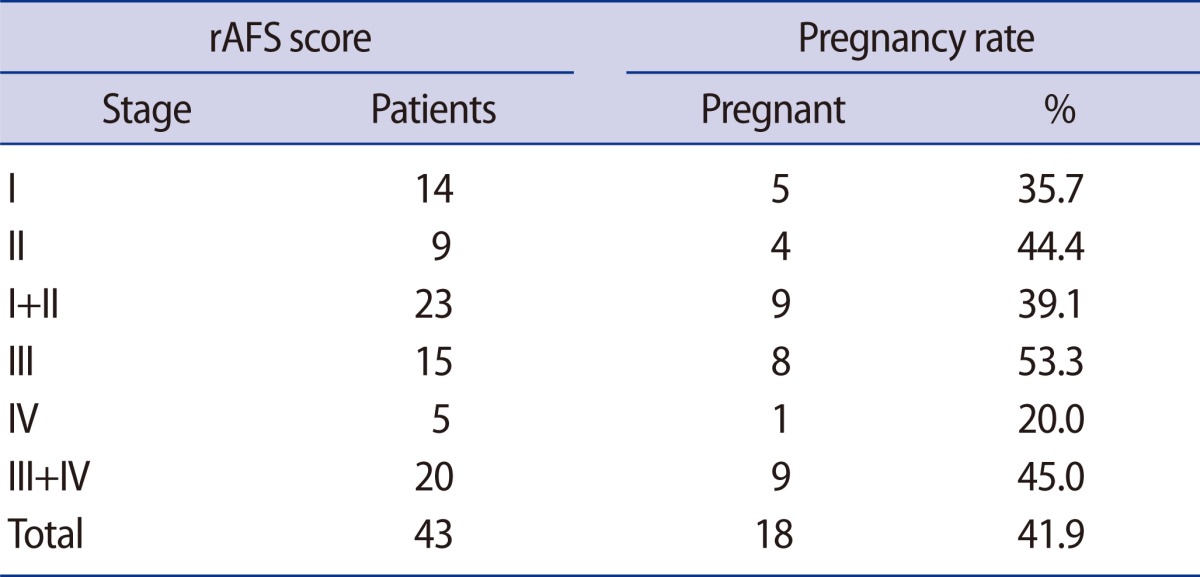
The pregnancy rates were 35.7%, 44.4%, 53.3%, and 20.0% for stage I, II, III, and IV, respectively (Table 2). Although there was no significant difference according to the AFS stages, the pregnancy rate for stage IV was relatively low (20.0%).
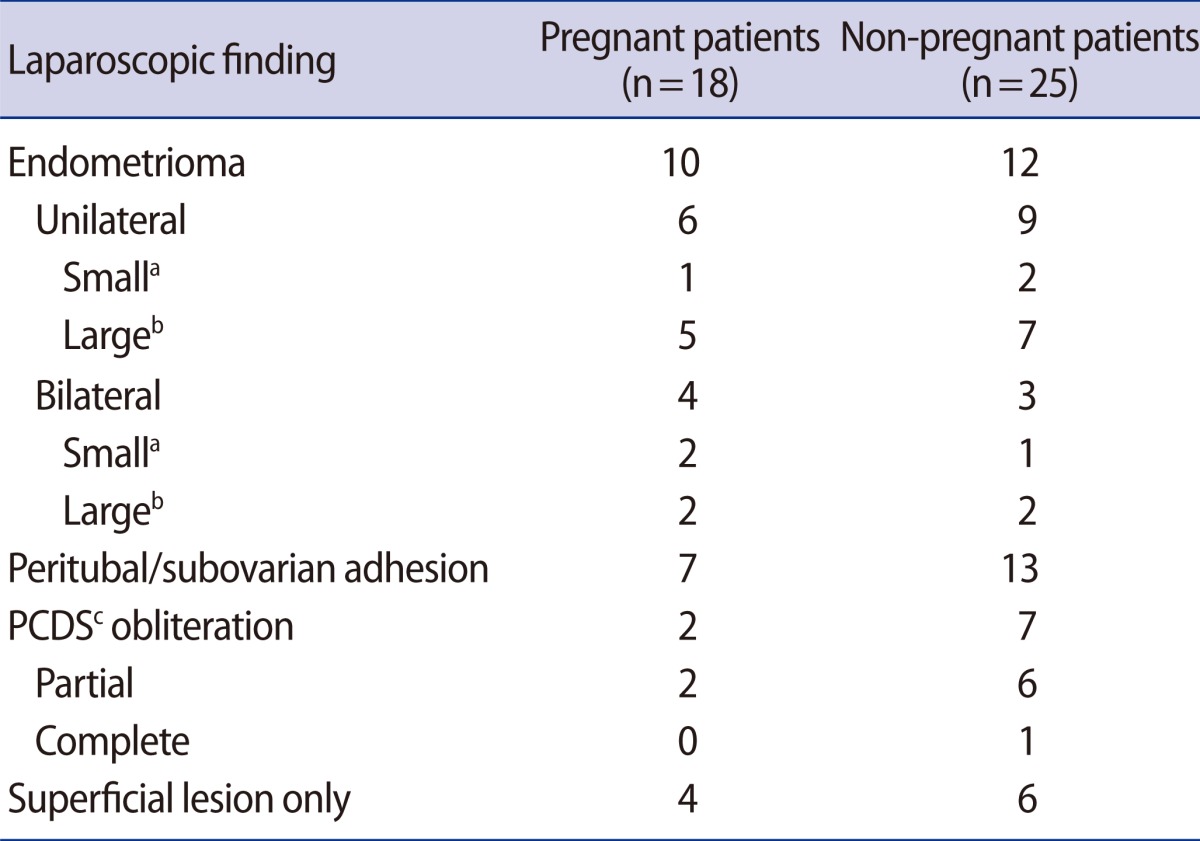
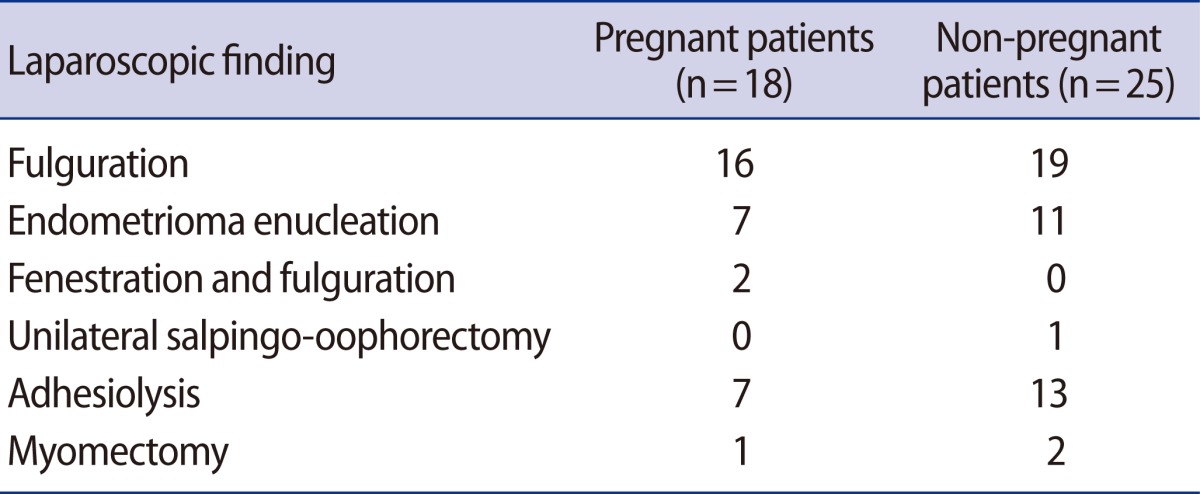
On laparoscopy, endometriomas were found in 22 patients, peritubal/subovarian adhesion in 20 patients, posterior cul-de-sac (PCDS) obliteration in 9 patients, and superficial lesions only in 10 patients. These findings as well as the types of surgery were not significantly different between the pregnant and non-pregnant group (Tables 3, 4).
Discussion
The association between endometriosis and infertility has been given much attention; however, the role of surgery in enhancing pregnancy rates remains elusive. In the present study, we retrospectively studied the natural conception rate of infertile women with endometriosis during one postoperative year and found that 41.9% of women successfully conceived without ART or hormone treatment.
To date, only two randomized controlled trials have studied whether laparoscopic surgical treatment of minimal and mild endometriosis yielded a higher pregnancy rate than diagnostic laparoscopy only. Marcoux et al. [4] reported that in the 36 weeks after laparoscopic resection or ablation of endometriosis, the cumulative pregnancy rate was 30.7%, compared with 17.7% in the controls. As a well-designed trial engaging 172 patients, it provided a solid level of evidence supporting surgery for early stage endometriosis. Gruppo Italiano, on the other hand, did not find a pregnancy rate in the resection/ablation group (24%) significantly different from the no treatment group (29%) [5]. As for deep infiltrating endometriosis, reported pregnancy rates range from 30% to 67%, with an overall weighted mean of about 50%, which has been considered to be an overestimate due to selection bias and publication bias [11].
Our data were in agreement with the aforementioned findings showing an average pregnancy rate of 41.9%, while the pregnancy rate for stage IV was lower than the average of the rest (stage I, 35.7%; stage II, 44.4%; stage III, 53.3%; and stage IV 20.0%). The pregnancy rates were not inversely proportional to the stages, which reflected the inadequate predictive value of the AFS staging system with regard to the pregnancy rate [12,13]. In order to overcome the limit of the current staging system, several predictive factors for the pregnancy rate in infertile patients with endometriosis have been suggested, such as complete cul-de-sac obliteration [14] and peritubal/ovarian adhesion [15,16]. In our study, it is noteworthy that the PCDS obliteration and peritubal/subovarian adhesion was more frequently shown in the not-pregnant group, as opposed to the presence of endometrioma. In stage IV, all of the four patients who failed to conceive had PCDS obliteration or peritubal/subovarian adhesion, whereas one patient who became pregnant did not. In addition, regardless of the stage, the not-pregnant group had more peritubal/subovarian adhesion and PCDS obliteration than the pregnant group, although it did not reach statistical difference partially due to the small number of patients. Further study on a larger number of patients is warranted to clarify the role of peritubal/subovarian adhesion and PCDS obliteration in endometriosis-caused infertility.
Accordingly, the need for radical interventions for rectovaginal lesions has been proposed; however, it is questioned whether the efficacy outstripped the risk of major complications such as ureteral and rectal injuries. Douay-Hauser et al. [17] observed that extensive surgery for deep endometriosis in infertile women did not modify the global fertility outcome but was associated with a higher complication rate. In addition, according to the review of Vercellini et al. [11], radical excision of rectovaginal endometriosis did not greatly improve reproductive prognosis.
In this study, most of the patients conceived within 6 months after the surgery, as has generally been reported [4,16]. Somigliana et al. [18] observed that delaying conception after surgery was associated with a lower pregnancy rate and a higher rate of recurrence of endometriosis. Thus, after a thorough analysis of the patients' reproductive status such as age, duration of infertility and other infertility causes, surgery and a prompt attempt at natural conception with sufficient time (at least six months) is advisable.
In conclusion, the present study shows that the natural conception rate was 41.9% during the first year after laparoscopic surgery in infertile women with endometriosis and no other factors. This information should be useful to infertile patients seeking treatment for endometriosis and the physicians counseling them.
Notes
This study was supported by a grant of the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (01-PJ10-PG6-01GN13-0002).
No potential conflict of interest relevant to this article was reported.