Fertility preservation for patients with gynecologic malignancies: The Korean Society for Fertility Preservation clinical guidelines
Article information
Abstract
Fertility preservation plays a central role in cancer care since an increasingly large number of cancer patients are surviving as a result of improvements in diagnostic and therapeutic strategies. Physicians who take part in the initial diagnosis and management of gynecologic cancer should understand the importance of fertility preservation. Since indications for fertility preservation are limited to early-stage gynecologic cancer, a surgeon must carefully consider each indication. Before performing fertility-sparing surgery, health professionals should compare its oncologic and pregnancy outcomes with those of other standard treatments. Individualized treatment strategies should be delivered depending on the patient's situation, and physicians should provide timely information and appropriate counseling.
Introduction
Standard guidelines for fertility preservation were first proposed in 2006 by the American Society of Clinical Oncology. Those guidelines recommended using gonadal shielding during radiotherapy to reduce the radiation doses delivered to reproductive organs and applying ovarian transposition (oophoropexy), in which ovaries are surgically displaced to avoid radiation damage, as standard methods of treatment. Trachelectomy, in which only the cervix is removed, and other conservative surgical treatments that avoid surgical removal of the ovaries are standard treatments for cervical and gynecologic cancer [1].
In 2012, the National Comprehensive Cancer Network (NCCN) proposed guidelines for adolescent and young adult oncology, which recommended that young patients aged 15 to 39 years with cancer be sufficiently informed about fertility preservation and the risk of infertility as a result of cancer treatment [2]. The present study reviews the methods of fertility preservation for patients with different types of gynecologic cancer: cervical cancer, ovarian cancer, and endometrial cancer.
Options for fertility preservation in gynecologic malignancies
1. Cervical cancer
According to the statistics reported by the National Cancer Registration and Statistics System, in 2012, 3,857 people developed cervical cancer, and cervical cancer was the seventh most common type of cancer among women in Korea. Of those affected by cervical cancer, 1,235 were younger than 46 years, and one-third of all cases of cervical cancer occurred among women of childbearing age [3].
As mentioned in the introduction, ovarian transposition is a standard practice for patients with cervical cancer who wish to preserve their fertility. In cases of locally confined cervical cancer, it is important to transpose the ovaries above the upper border of the target radiation field. In general, the upper border of the radiation field is defined as the upper border of the L4/L5 lumbar vertebra. During standard ovarian transposition, the ovaries should be surgically moved to above the anterior superior iliac spine or up to the navel to prevent them from undergoing radiation damage [45].
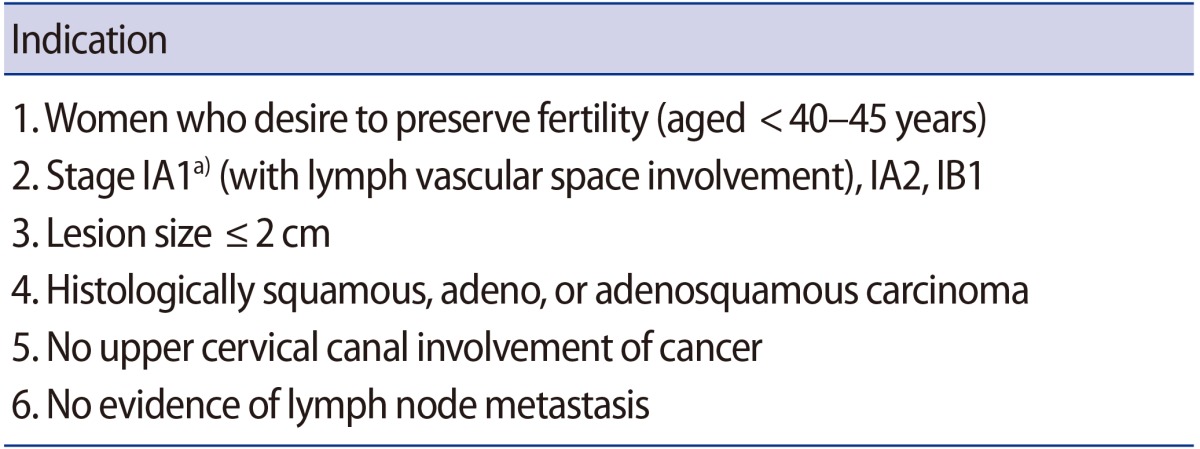
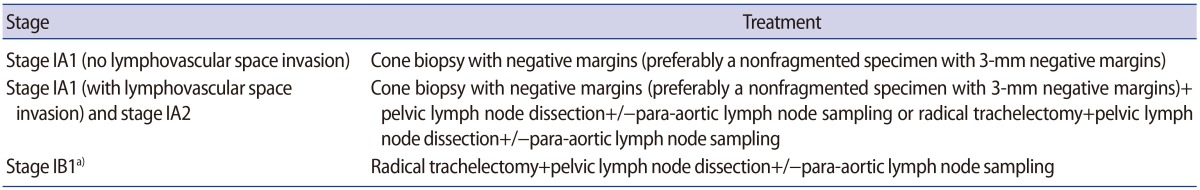
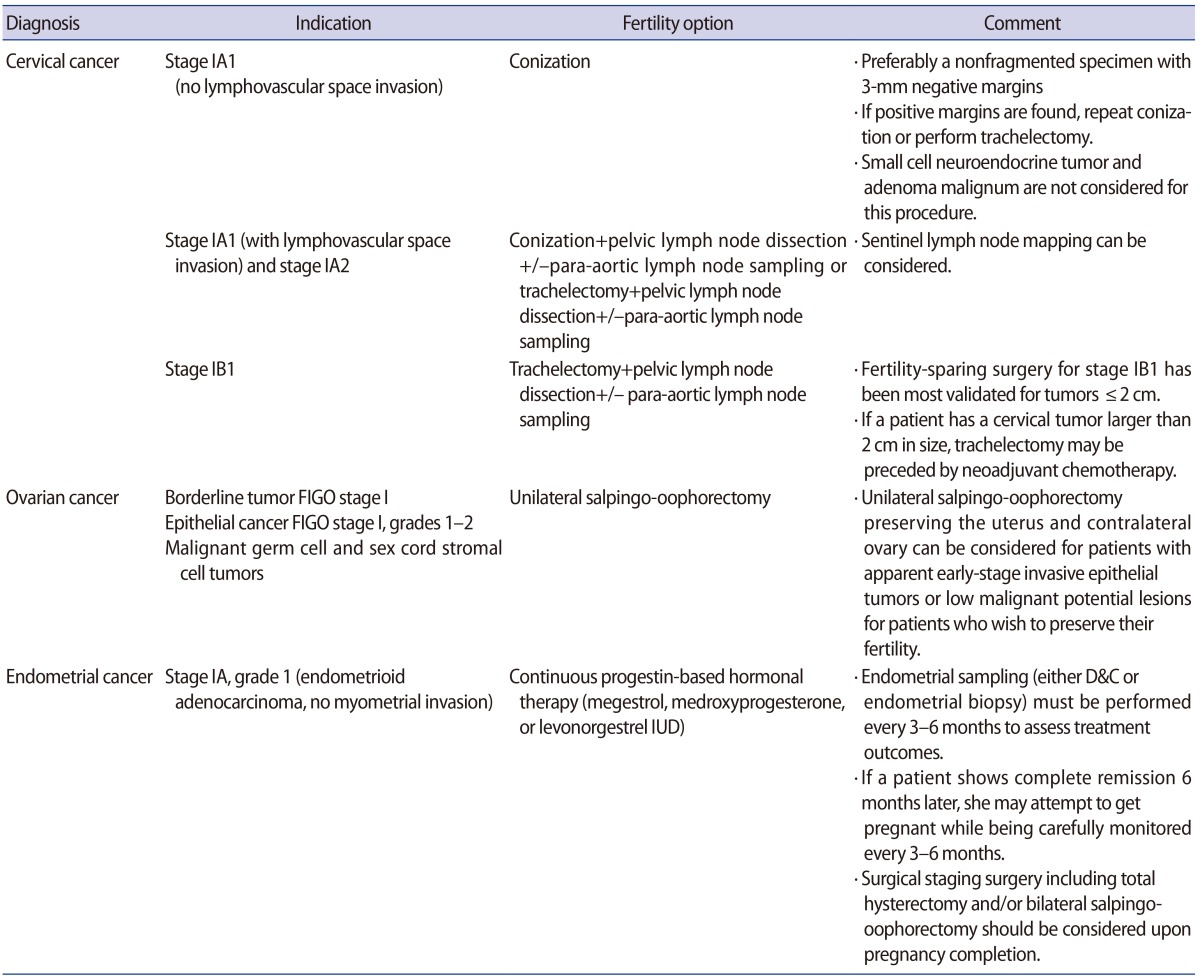
Conization and trachelectomy are standard methods of fertility preservation for patients with early-stage cervical cancer. The indications for trachelectomy are presented in Table 1 [4]. Cervical conization can be performed for stage IA1 or IA2 cervical cancer. The indications for fertility-sparing surgery in cervical cancer proposed by the NCCN guidelines are listed in Table 2 [6].
The oncologic outcomes and obstetric outcomes of trachelectomy are as follows. In the combined results of multiple studies, the rate of recurrent cervical cancer was 3.5% (22 of 619) and that of mortality was 1.9% (12 of 619) in a total of 619 patients with cervical cancer who underwent trachelectomy. Among the 619 patients, 236 patients successfully became pregnant, but 20% of these patients had a miscarriage in the first trimester, and 8% (20 of 236) had a miscarriage in the second trimester. Eventually, 66% of the pregnant patients had a delivery in the third trimester (157 of 236), 15% before the 32nd week of pregnancy and 85% after the 32nd week of pregnancy [7891011].
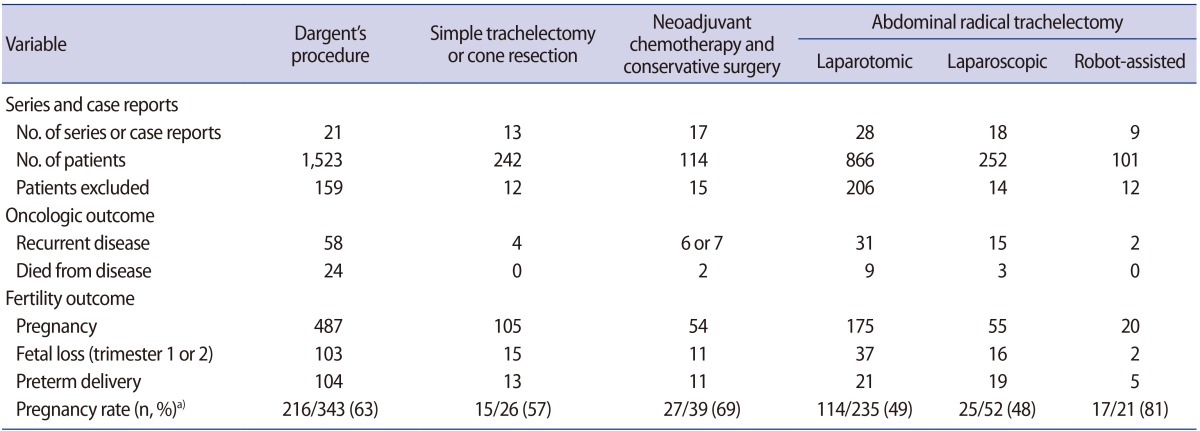
If a patient has a cervical tumor larger than 2 cm, trachelectomy may be preceded by neoadjuvant chemotherapy, which is performed to reduce the size of the tumor. In a study that investigated the oncologic outcomes of neoadjuvant chemotherapy followed by trachelectomy in 54 patients, a complete or partial response was observed in 81.5% of the patients (44 of 54); recurrence occurred in three patients; and 28 patients successfully became pregnant [12]. In a recent systemic review, six different techniques of trachelectomy were assessed in terms of oncologic and pregnancy outcomes (Table 3). The authors recommended that fertility preservation techniques should be selected based on the experience of the team, discussion with the patient or couple, and objective oncologic data to balance the best choice for a cure with the optimum fertility results [1314].
2. Ovarian cancer
Ovarian cancer can be categorized as benign, borderline, and malignant tumors. Since conservative surgery is performed in most women of childbearing age with benign tumors, we would like to focus our discussion on borderline and malignant tumors.
1) Borderline tumors
Borderline tumors have excellent prognoses. For stage 1 ovarian cancer, the 15-year survival rate is 98%. Even with all cancer stages included, the 5-year survival rate of borderline ovarian cancer is 86% to 90% (American Cancer Society, National Cancer Institute, SEER [Surveillance, Epidemiology, and End Results] data 2004 to 2010). In a meta-analysis that included 39 studies and a total of 5,105 patients who underwent conservative surgery for borderline tumors, the rate of recurrence was lower for patients who underwent unilateral salpingo-oophorectomy than for those who underwent ovarian cystectomy. However, no significant difference in the survival rate was found between the two groups of patients [15].
The NCCN guidelines also recommend that unilateral salpingo-oophorectomy preserving the uterus and contralateral ovary can be considered for patients with apparent early-stage invasive epithelial tumors or low malignant potential lesions who wish to preserve their fertility. Chemotherapy is not recommended because it has no known benefits in the treatment of borderline tumors.
Studies have reported no difference in the pregnancy rates between patients who have a single ovary after undergoing unilateral salpingo-oophorectomy and those with two ovaries. However, differences in the length of pregnancy between these groups have been reported [16].
2) Malignant tumors
Epithelial ovarian cancer represents 80% of all malignant ovarian tumors and is the most common type of ovarian cancer. Surgical staging and/or cytoreductive surgery followed by adjuvant chemotherapy are performed as the primary treatment of ovarian cancer. The complete surgical staging includes peritoneal and pelvic washing cytology, total hysterectomy, bilateral salpingo-oophorectomy, omentectomy, pelvic/para-aortic lymphadenectomy, and multiple peritoneal biopsies.
According to the clinical practice guidelines for gynecologic cancer published by the Korean Gynecologic Oncology Group, patients who exhibit stage IA or IC cancer based on surgical findings, and who wish to become pregnant in the future, can undergo fertility-preserving surgery, in conjunction with comprehensive surgical staging, regardless of the cancer grade [17181920].
Comprehensive surgical staging is a replacement procedure for complete surgical staging, and it includes preservation of the uterus and an ovary at the operating surgeon's discretion, as well as a thorough gross and broad histological examination of all intraperitoneal and retroperitoneal organs. The NCCN guidelines recommend chemotherapy for stage IC cancer regardless of the cancer grade, as well as for stage IA or IB cancer with grade 3 tumors or clear cell adenocarcinoma [21]. Using a stricter standard, some studies have recommended that stage IA or IB and grade 1 or 2 cancer be used as an appropriate indication for fertility preservation [2223]. Park et al. [24] investigated the oncologic safety and reproductive outcomes of fertility-preserving surgery in patients with epithelial ovarian cancer in Korea, and reported low survival rates for patients with cancer at higher than stage IC or at grade 3, and concluded that stage IA–C and grade 1–2 cancer can be safely treated with fertility preservation.
Regarding germ cell tumors and sex-cord stromal cell tumors, stage IA/IB dysgerminomas, stage IA grade 1 immature teratomas, and stage IA embryonal or yolk sac tumors can be monitored clinically without the use of chemotherapy for fertility preservation.
Ovarian carcinosarcoma is a rare type of cancer, and has a poor prognosis according to the NCCN guidelines. Fertility preservation treatment is not recommended regardless of the patient's age [21].
3. Endometrial cancer
Endometrial cancer is the most common gynecologic malignancy in Western countries, and it has steadily increasing recently in Korea. Approximately 3% to 14% of endometrial cancer cases are diagnosed in premenopausal women 40 years of age or younger who want to preserve their fertility [2526272829].
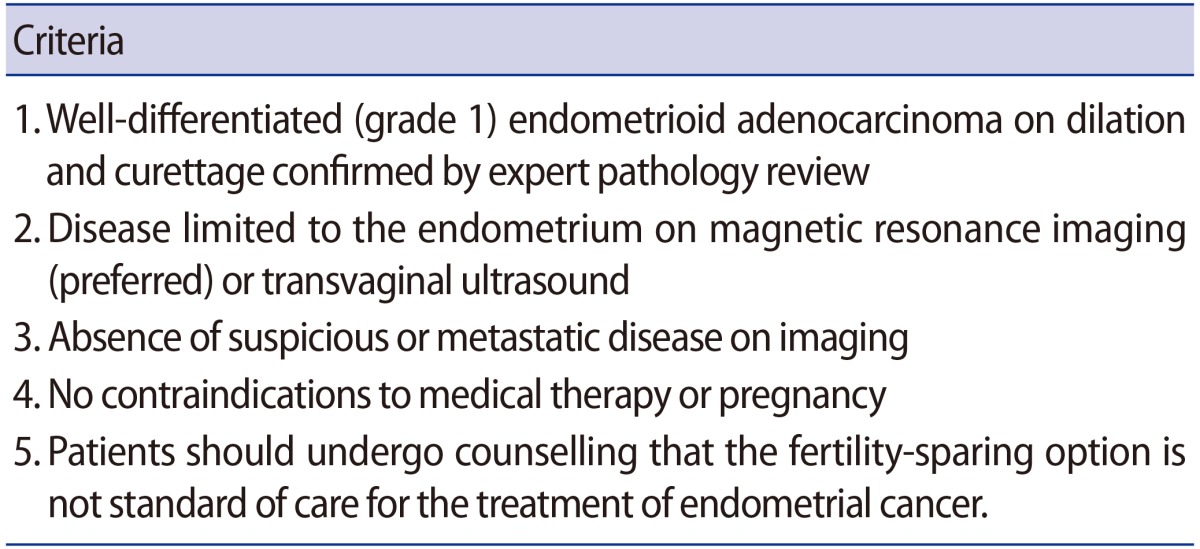
According to clinical practice guidelines for gynecologic cancer, total hysterectomy, bilateral salpingo oophorectomy, pelvic/para-aortic lymphadenectomy, and pelvic/peritoneal washing cytology are performed as the standard primary procedures for the surgical staging of endometrial cancer [30]. The NCCN guidelines advise that fertility preservation be considered only when all the following conditions are met (Table 4) [31].
Fertility-preserving surgery can be performed when there is no invasion into the myometrium by stage I grade 1 endometrial cancer. For patients who satisfy all the aforementioned conditions, the use of megestrol, medroxyprogesterone, or a levonorgestrel intrauterine device (IUD) can be considered for continuous progestin-based therapy. According to the literature, the appropriate dose of megestrol is 40–400 mg/day, and that of medroxyprogesterone is 200–800 mg/day [323334]. Following continuous progestin-based therapy, endometrial sampling, either through dilation and curettage or endometrial biopsy, must be performed every 3–6 months to assess treatment outcomes. Patients who had an IUD inserted may experience discomfort during IUD replacement at each assessment. If a patient shows complete remission 6 months later, she may attempt to get pregnant while being carefully monitored every 3–6 months, and undergo surgical staging surgery, including total hysterectomy and/or bilateral salpingo-oophorectomy, upon pregnancy completion.
Oophorectomy is commonly performed in premenopausal women with endometrial cancer; however, many studies found that ovarian preservation had no effect on the overall survival of young patients with early-stage endometrial cancer. Ovarian preservation is likely to be safe and not associated with an increase in cancer-related mortality [353637].
If the patient does not become pregnant during the monitoring period and develops new or recurrent endometrial cancer, she must consider undergoing surgical staging surgery. If endometrial cancer is detected within 6–9 months after the completion of the aforementioned medical therapies and the assessment of treatment outcomes, surgical staging surgery must again be considered.
In regard to the oncologic and pregnancy outcomes of fertility-sparing therapies, a systematic review and meta-analysis performed by Gallos et al. [38] found the regression rate of endometrial cancer to be 76.2%, the relapse rate to be 40.5%, and the live birth rate to be 28% following fertility-preserving surgery.
Conclusion
Fertility-sparing options in the treatment of gynecologic malignancies are summarized in Table 5. Health professionals must discuss the risk of early menopause and infertility with patients of childbearing age and their families. Before performing fertility-preserving surgery, health professionals should compare its oncologic and pregnancy outcomes with those of other standard treatments. In addition, since indications for fertility preservation are limited to early-stage gynecologic cancer, a surgeon must carefully consider each indication and be aware that fertility-preserving surgery should be performed only when treatment options are limited to conservative treatment or pharmacotherapy.
Notes
*This study was supported by the National Research Foundation of Korea Grant funded by the Korean Government (No. NRF-2016R1C1B3015250).
Conflict of interest: No potential conflict of interest relevant to this article was reported.