Multiple pregnancy after single or multiple embryo transfer performed according to Korean guidelines
Article information
Abstract
Objective
To assess compliance with Korean guidelines for embryo transfer, the possible reasons for non-compliance, and multiple pregnancies according to each specific condition in compliant cycles.
Methods
A single-institution, retrospective study was conducted of 256 fresh in vitro fertilization cycles during 2012-2014. To assess compliance with Korean guidelines, the maximum recommended number of embryos transferred (according to criteria of age, transfer day, and presence of favorable conditions) was compared with the actual number of embryos transferred. Clinical pregnancy rate (PR) was assessed as the percentage of pregnant women resulting from each set of transfer conditions, including the number of embryos transferred. The multiple pregnancy rate (MPR) was calculated as the percentage of pregnant women with a multifetal pregnancy.
Results
The compliance rate with the Korean guidelines was 96.5% (247/256). Non-compliance occurred in nine cycles owing to poor embryo quality, repeated implantation failure, or hostile endometrium. In compliant cycles, the PR was 31.2% (77/247), and the MPR was 27.3% (21/77; 20 twins and one triplet). Higher MPR was noted in two types of transfer conditions: transfer of three cleavage embryos in women aged 35-39 years with favorable conditions (66.7%; primarily from those aged 35-37 years) and transfer of two blastocysts in women aged ≥40 years with favorable conditions (50%).
Conclusion
Under the Korean guidelines, compliance rate was high in our center. Multiple pregnancies occurred primarily in group with favorable conditions. In high-risk groups for multiple pregnancies, reducing number of embryos transferred should be considered than suggested in the guideline.
Introduction
In the past 20 years, multifetal births have increased 1.9-fold in Korea and continue to increase steadily, a change that is attributed to the increasing use of assisted reproductive technology [12]. In medically assisted reproduction, multiple ovulation induced by ovarian stimulation and multiple embryo transfer in in vitro fertilization (IVF) cycles commonly result in multifetal pregnancy. It is well known that multifetal pregnancies can cause obstetric complications such as preterm births and low birth weight, thus increasing maternal and fetal morbidity and mortality [3]. In a recent meta-analysis, multifetal pregnancies generated by assisted reproduction were associated with higher risks of pregnancy-related complications and adverse pregnancy outcomes than those arising from spontaneous conception [4].
The issues regarding multifetal pregnancy in IVF cycles have been emerging since the late 1990's from Europe and Australia. Several countries have law or guidelines to regulate the number of embryos transferred. In USA, guidelines for the number of embryos transferred were established in 1998 by the American Society for Reproductive Medicine/Society for Assisted Reproductive Technology (ASRM/SART) and revised in 2004 [5]. According to these guidelines, the number of embryos transferred depends on three criteria: maternal age, transfer day, and the presence of favorable conditions [5]. The USA guidelines were further revised in 2006 by the addition of criteria for blastocyst transfer [6], but the number of embryos transferred remained unchanged in the most recently published revision in 2013 (Table 1) [7].
In Korea, guidelines for the number of embryos transferred were established in 2008 by the government. The three criteria and four favorable conditions are similar to those in the USA guidelines (Table 1), but with differences as follows: (1) maternal age is divided into three groups (compared to four in the USA); (2) a maximum recommended number of three cleavage embryos is transferred in women aged <35 years with non-favorable conditions (compared to two embryos in the USA), or two blastocysts with favorable conditions (compared to one in the USA); and (3) the maximum recommended numbers of embryos transferred in women aged 35-39 years is the same as that in American women aged 38-40 years (i.e., one additional embryo can be transferred in Korean women aged 35-37 years than in American women of this age).
Taken together, the recommended maximum number of embryos transferred according to the Korean guidelines is higher than in the USA guidelines. The present study aimed to investigate whether the Korean guidelines are appropriate for reducing the number of multiple pregnancies. The frequency of compliant cycles was assessed and the reasons for non-compliance were explored. In compliant cycles, the pregnancy rate (PR) and multiple pregnancy rate (MPR) were assessed according to each transfer condition.
Methods
A single-institution, retrospective study was conducted at the Seoul National University Bundang Hospital with the approval of the Institutional Review Board. Two hundred and fifty-six fresh IVF cycles with embryo transfer performed between 2012 and 2014 were identified. Patient demographics and clinical characteristics were collected through electronic medical records, which included maternal age, parity, cycle number, transfer day, and number of embryos transferred.
Information on embryo quality assessed by cell number and grade was also collected. The grade of embryo was evaluated using morphological criteria, based on the degree of fragmentation and the regularity of blastomeres, as follows: grade A, equal-sized blastomeres and no fragments or apparent morphologic abnormalities; grade B, equal-sized blastomeres and <20% of fragments without apparent morphologic abnormalities; grade C, irregularity of blastomeres and 20%-50% of fragments without apparent morphologic abnormalities; grade D, irregularity of blastomeres and >50% fragments with apparent morphologic abnormalities.
Clinical pregnancy was defined as the detection of identifiable intrauterine gestational sac(s) with fetal heartbeat(s), and PR was calculated as the percentage of pregnant women per transfer cycle. Multifetal pregnancy was defined as the detection of ≥2 intrauterine gestational sacs with fetal heartbeats, and the MPR was calculated as the percentage of pregnant women with multifetal pregnancy. The initial number of gestational sac(s) was always used in analysis, although subsequent miscarriage or vanishing twin sometimes occurred.
The maximum recommended number of embryos transferred was assessed and compared to the actual number of embryos transferred, and compliance or non-compliance with the recommendation was determined. In non-compliant cycles, the reasons for noncompliance and the occurrence of any resultant pregnancy were recorded. In compliant cycles, PR and MPR were assessed according to each specific transfer condition and the number of embryos transferred. The present study was a simple descriptive study; therefore, no statistical analysis was needed.
Results
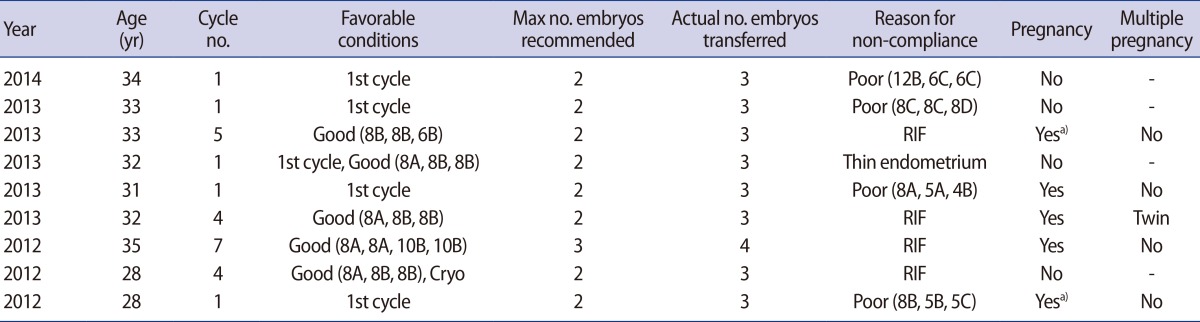
At our institution, 256 fresh IVF cycles were performed from 2012-2014. The compliance rate was 96.5% (247/256), with non-compliance in nine cycles. Reasons for non-compliance were poor embryo quality in four cycles, repeated implantation failure in four cycles, and hostile endometrium in one cycle (Table 2). In the non-compliant group, five pregnancies occurred (PR=55.6%) and one twin pregnancy was identified among these (MPR=20%).
In the compliant group (247 cycles), the mean age of the women was 35.9 years and the mean number of embryos transferred was two (one embryo in 60 cycles, two in 150 cycles, three in 31 cycles, and four in 6 cycles). Day 2 transfer was performed in two cycles, day 3 transfer in 196 cycles, day 4 transfer in one cycle, and day 5 transfer in 48 cycles. The overall PR in the compliant group was 31.2% (77/247), the MPR was 27.3% (21/77; 20 twins and 1 triplet), and the implantation rate was 20.8% (99/477). Spontaneous miscarriage was identified in 17 women (miscarriage rate=22.1% [17/77]).
One case of triplet pregnancy occurred in a 36-year-old, nulliparous woman. She underwent her second IVF cycle and good quality embryos were obtained (one 8-cell embryo of grade A and two 8-cell embryos of grade B); thus, the maximum recommended number of embryos was three at day 3. Three embryos were transferred at day 3 (compliant cycle), and a triplet pregnancy was subsequently noted. She underwent selective fetal reduction and the resulting twins were delivered via cesarean section.
Table 3 shows the PR and MPR according to the number of embryos transferred, irrespective of age and transfer day. Interestingly, twin pregnancies also occurred after single embryo transfer (MPR=6.7%).
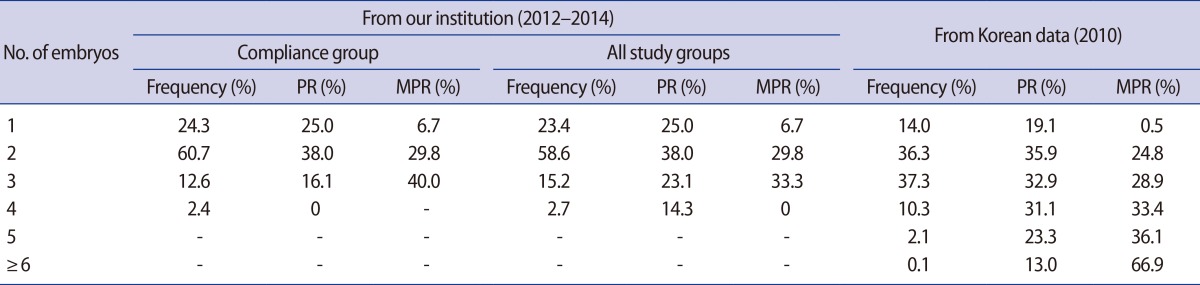
Frequency of number of embryos transferred, PR, and MPR from our institution and from Korean registry data
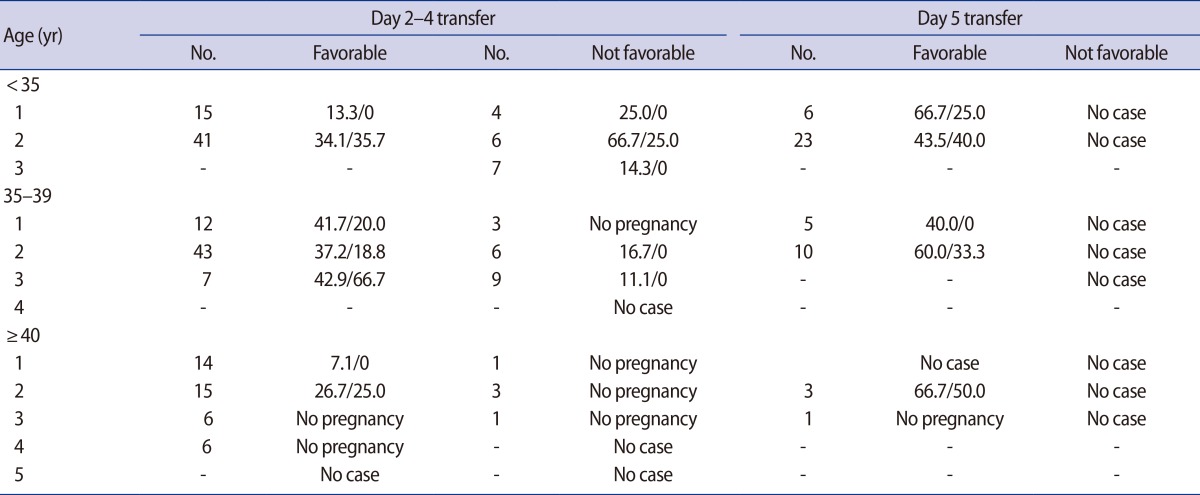
Table 4 shows the PR and MPR for each transfer condition in the compliant group (247 cycles). Higher MPR was noted in two situations with the presence of favorable conditions: transfer of three cleavage embryos in women aged 35-39 years (66.7%) and transfer of two blastocysts in women aged ≥40 years (50%).
When the group aged 35-39 years was divided into those aged 35-37 years and 38-39 years, multiple pregnancies from transfer of three cleavage embryos and transfer of two blastocysts were only seen in the group aged 35-37 years (Table 5). Under the same transfer conditions, no pregnancies occurred in the group aged 38-39 years.
Discussion
Regulation of the number of embryos for transfer primarily aims to reduce high-order multifetal births. In our study, only one triplet pregnancy was noted in all cycles, including the compliant and non-compliant groups; clinical pregnancies occurred in 82 cycles (PR=32.0%), including 21 twin and 1 triplet pregnancy (MPR=26.8%). Although non-compliance with the transfer guidelines occurred in nine cycles, the PR and the frequency of high-order multiple pregnancy were acceptable. Moreover, selective fetal reduction was performed in the one triplet case, thus multi-fetal births larger than twin births did not occur.
Higher MPR was noted in two situations in the present study; transfer of three cleavage embryos in women aged 35-39 years (66.7%) and transfer of two blastocysts in women aged ≥40 years. Therefore, it would be reasonable to reduce the number of embryos for transfer than suggested by the guideline in such situations.
Women aged <35 years old are a high-risk group for high-order multiple pregnancy. In the Korean guidelines, one additional embryo is permitted to be transferred in women aged <35 years, both in day 2-4 transfer of with non-favorable conditions and in day 5-6 transfer with favorable conditions, compared to the USA guidelines. Under these conditions in our population, the MPR was acceptable; thus, reducing the number of embryos for transfer appears to be unnecessary. However, transfer of two blastocysts in women aged <35 years with favorable conditions (compliant group) yielded a rather high MPR (40%); therefore, single blastocyst transfer should be considered in that situation.
Maternal age is divided into four groups in the USA guidelines, but in the Korean guidelines, there are only three age groups. The maximum recommended numbers of embryos for transfer in Korean women aged 35-39 years is the same as that in American women aged 38-40 years; thus, one additional embryo can be transferred in Korean women aged 35-37 years. Therefore, according to the Korean guidelines, a higher MPR would be expected in Korean women aged 35-37 years; this was noted to be the case in the present study. The MPR was 66.7% following transfer of three cleavage embryos in women aged 35-39 years with favorable conditions and multiple pregnancies exclusively emerged from women aged 35-37 years. Therefore, clinicians should consider reducing number of embryos transferred than suggested in the guideline, especially when woman is 35-37 years.
In the USA, an average of two embryos was transferred per cycle in 2010, and the average number of embryos transferred increased with age (2.0 among women aged <35 years, 2.4 among women aged 35-40 years, and 3.0 among women aged >40 years) [9]. In this report, there was a substantial proportion (43.4%) of twin pregnancies, and a smaller proportion (3.0%) of triplets or higher order pregnancies. After the publication of the ASRM/SART embryo transfer guidelines, a significant decrease in the number of embryos transferred and multifetal births was reported in the USA [1011].
In Europe, despite huge differences in embryo transfer policy between countries, the overall trend seen over the last 10 years towards transferring fewer embryos appears to be continuing [12]. In Europe, the most frequent ET number was two between 2008 and 2010, and the percentages of cycles where ≤2 embryos were transferred were 75.6% in 2008, 81.9% in 2009, and 82.4% in 2010 [12]. Among live births, multifetal birth rates were 21.7% in 2008, 20.2% in 2009, and 20.6% in 2010.
In Korea, the embryo transfer number between 2007 and 2008 was mostly three or four [1314], but this decreased to two or three between 2009 and 2010 [18]. Multifetal birth rates were 50.1% in 2007, 52.2% in 2008, and 46.5% in 2009, falling to 25.6% in 2010 [181314]. The triplet or high-order birth rate was 0.7% in 2007, 1.5% in 2008, 1.2% in 2009, and 0.6% in 2010. This dramatic decrease in multifetal births in Korea might be due to good compliance with the guidelines for embryo transfer. However, the most frequent transfer number was two or three (overall mean=2.5) and the percentage of cycles in which ≤2 embryos were transferred was 50.3% in 2010, a figure that was lower than in Europe.
In the 2013 USA guidelines, in each of the above age groups for patients with ≥2 previous failed fresh IVF cycles or a less favorable prognosis, one additional embryo may be transferred according to individual circumstances [7]. Such documentation is absent in the Korean guidelines, but a statement about clear documentation is included: "Justification for transferring one additional embryo more than the recommended limit should be clearly documented in the patient's medical record." In our study, non-compliance mostly occurred in women with poor embryo quality or repeated implantation failure. Therefore, it is reasonable that one additional embryo is allowed in several exceptional situations, especially in women with a poor prognosis.
In the USA, programs that have a high-order multiple pregnancy (≥3 implanted embryos) rate that is >2 standard deviations above the mean rate for all SART-reporting clinics, for two consecutive years, may be audited by SART [7]. In Korea, compliance with the guidelines or managing the incidence of high-order multiple pregnancy is not presently regulated.
Reducing the embryo number for transfer is an obvious strategy to reduce high-order multifetal births. As shown in Korean data from 2010, a maximum PR and minimal MPR can be obtained with the transfer of two, rather than three embryos. Therefore, the majority of cases should have two embryos transferred. Reducing the number of embryos transferred in groups at high risk of high-order multiple pregnancy and promotion of elective single embryo transfer is needed to reduce multiple births and the related adverse events of assisted reproductive technology. We recognize that the present study comes from a single institution; thus, further nationwide surveillance is needed to identify groups at high risk of high-order multiple pregnancy.
Notes
This work was supported by a grant (No. A120043) from the Korea Health Care Technology R&D Project, Ministry of Health and Welfare, Korea.
Conflict of interest: No potential conflict of interest relevant to this article was reported.