|
 |
- Search
| Clin Exp Reprod Med > Volume 41(4); 2014 > Article |
Abstract
Objective
The objective of this study is to estimate the effects of Inclear, a feminine cleanser, on sperm motility.
Methods
Semen samples were obtained from infertile male patients. Following liquefaction, the raw semen samples were diluted with Ham's F-10 nutrient mixture medium containing 0.4% human serum albumin solution at a ratio of 1:3. The semen samples were subsequently centrifuged to separate the seminal plasma from the serum. The supernatant was discarded, and the pellet was resuspended. The sample was again centrifuged to remove cell debris, and the supernatant was removed. The final pellet was gently loosened by resuspension and incubated in medium alone as a control, and in a 10% solution of the medium plus Inclear. A sampling time of 30 minutes was selected on the basis of sperm transport studies. Sperm motility was evaluated with computer-assisted sperm analysis.
Results
A total of 20 samples were analyzed. The mean age of patients was 34.40┬▒2.96 years. There was no difference in sperm concentration and motility in the two samples at 0 minute and 30 minutes of incubation. In both semen samples, the sperm concentration and motility decreased after an incubation period of 30 minutes. However, there was no statistical difference between the samples. Sperm concentration and motility were not significantly different between the control and Inclear samples after 0 minute and 30 minutes of incubation.
Vaginal lubricants are commonly used to reduce pain or dryness during intercourse [1]. In the United States, 62% of women have used a lubricant at some point during sexual activities, and 25.3% have used a lubricant within the previous month [2]. A more recent study by Herbenick et al. [3], which surveys the usage of vaginal lubricants, reports that 65.5% (n=1,021) of women have used lubricants, and that 20% used a lubricant within the past 30 days. Across age groups, lubricants are most commonly used during intercourse (58.3% of women report using them during sex) or other partnered sexual activity (49.6%). Common reasons for lubricant use include efforts to make sex more comfortable, fun, and pleasurable, and to decrease discomfort or pain.
Previous studies have reported that commonly used vaginal lubricants have been shown to negatively affect sperm motility in vitro [1,4,5,6]. One study showed that the usage of lubricants during procreative intercourse does not appear to reduce the probability of conceiving [7], while the majority of in vitro studies show that lubricants diminish sperm motility.
When trying to conceive, most couples have experienced vaginal dryness at some point during ovulatory intercourse due to having timed intercourse repeatedly on days around ovulation, the fear of failing at conception, and fertility medications. Twenty-five percent of these couples who are trying to conceive report always using a vaginal lubricant during intercourse [1].
Vaginal lubricant may be helpful to couples with sexual dysfunction such as vaginal dryness or pain during intercourse when trying to conceive.
The objective of this study is to identify the effects of Inclear, a new vaginal lubricant product, on sperm motility and mobility.
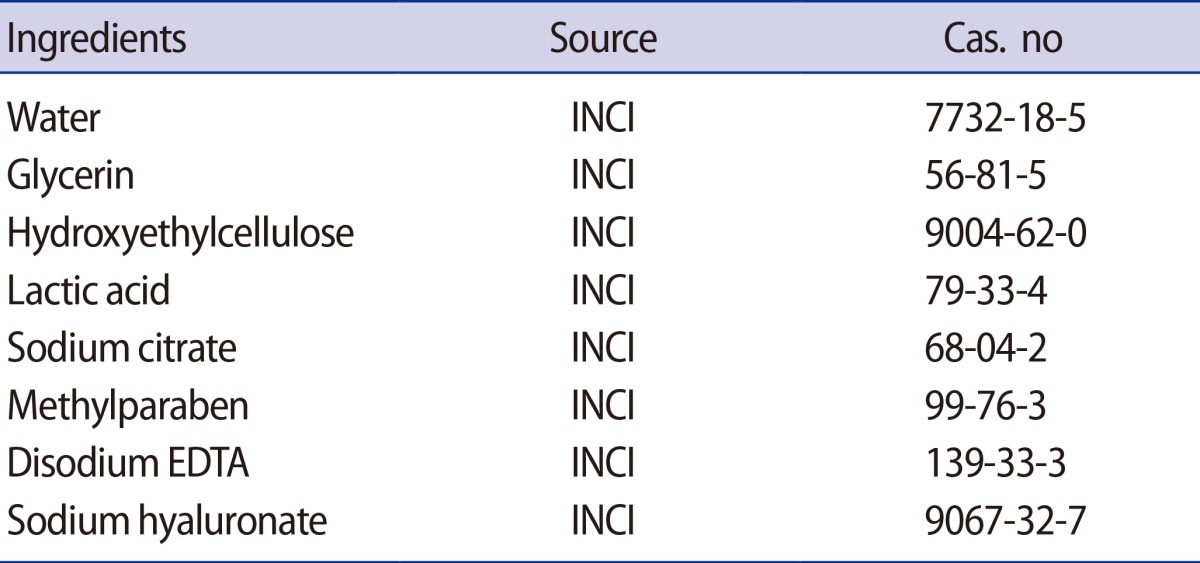
Semen samples were obtained from infertile male patients who had normal semen parameters. The semen samples were taken by masturbation following 3-5 days of abstinence, and collected in a sterile plastic container. After liquefaction for 30 minutes, the raw semen samples were diluted with Ham's F-10 nutrient mixture medium, containing 0.4% human serum albumin (HAS) solution at a ratio of 1:3. The tubes were placed in centrifuges, and the semen samples were subsequently centrifuged for 5 minutes at 1,460 rpm to separate the seminal plasma from the serum. The supernatant was discarded, and the pellet was resuspended in 1 mL of Ham's F-10 medium with 0.4% HAS solution. The sample was again centrifuged for 5 minutes at 1,460 rpm, and the supernatant was again removed. The final pellet was gently loosened by resuspension and incubated for 30 minutes at 37Ōäā under 5% CO2 in the medium alone as a control, and in 10% solutions of the medium plus Inclear. The major ingredients of Inclear are water, glycerin, hydroxyethylcellulose, sodium citrate, and lactic acid, with other ingredients in smaller proportions (Table 1). The 10% lubricant dilution was chosen on the basis of concentrations of lubricant potentially present after intercourse and ejaculation and has been used in previously published studies [1]. A sampling time of 30 minutes was selected on the basis of sperm transport studies. Sperm motility was evaluated with computer-assisted sperm analysis (CASA). The 30-minute sampling time was chosen on the basis of sperm transport studies suggesting that the majority of fertilizing spermatozoa migrate through the cervix within 15 to 30 minutes after ejaculation [8].
The study protocol was approved by the Institutional Review Board at Cheil General Hospital. Informed consent was obtained from the patients before obtaining semen samples.
Data are expressed as mean values┬▒SD. Sperm motility before and after incubation in each group was evaluated for statistically significant differences using a paired t-test or Wilcoxon signed rank test. Motility was evaluated between groups for statistically significant differences using Student's t-test or the Mann-Whitney test. A value of p<0.05 was considered statistically significant. Statistical analyses were processed using PASW ver. 18 (SPSS Inc., Chicago, IL, USA).
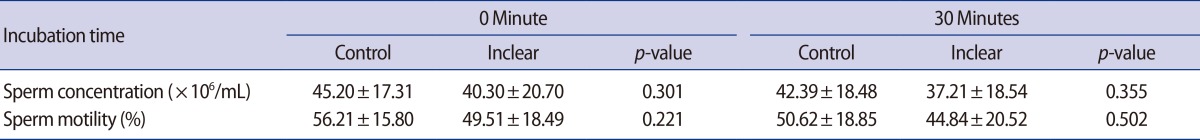
A total of 22 patients were enrolled in this study. Two patients were excluded from the study because of azoospermia. The mean age of the patients was 34.40┬▒2.96 years. There was no difference in sperm concentration and motility in the two samples after 0 minute and 30 minutes of incubation. In both semen samples, sperm motility decreased after 30 minutes of incubation. However, there was no statistical difference between the samples. Sperm concentration and motility were not significantly different between the control and Inclear samples after 0 minutes and 30 minutes of incubation (Table 2).
Many women use feminine hygiene products. Feminine hygiene products or methods may upset the normal pH level of approximately 4.5 in the vagina, which is important for maintaining a healthy vaginal environment and natural immunity [9]. Inclear was designed and introduced as a feminine hygiene product meant to improve vaginal pH levels, and to reduce odor and minimize irregular excreta from the vagina. The major ingredients of Inclear are water, glycerin, hydroxyethylcellulose, sodium citrate, and lactic acid, among other ingredients (Table 1). The glycerin in Inclear is commonly used as a main ingredient in many vaginal lubricants [10]. Thus Inclear may also be used as a vaginal lubricant to promote healthy and comfortable sexual activity.
Couples who are trying to conceive often use vaginal lubricants to make intercourse more comfortable. The effects of vaginal lubricants on sperm, however, can reduce a couple's chances of successful conception. Indeed, even when these products contain no spermicides, vaginal lubricants can have negative effects on sperm functions such as motility and mobility [6].
The present study tests whether the feminine hygiene product Inclear has negative effects on sperm motility when used as a vaginal lubricant.
As shown in Table 1, after incubating sperm for 30 minutes with Inclear, the product did not affect sperm motility (50.62┬▒18.85 vs. 44.84┬▒20.52; p=0.502). Among the motile sperm, motility changes differed according to their speed (rapid, medium, and slow on CASA). Thus, the motility of sperm may have been differentially affected by the viscosity of lubricant depending on their speed (Table 2). This data suggests that the number of fast, linear-moving sperm was not affected by Inclear after 30 minutes of incubation, and that the viscosity of Inclear is within a range that is conducive to sperm motility. In addition, we tested changes in sperm motility between the two groups, because sperm motility can be affected by chemicals that are external to spermatozoa [11,12,13].
In conclusion, this study finds that Inclear has no negative effects on sperm motility. Pregnancy planners with sexual dysfunction can use this product for vaginal hygiene and as a vaginal lubricant.
References
1. Agarwal A, Deepinder F, Cocuzza M, Short RA, Evenson DP. Effect of vaginal lubricants on sperm motility and chromatin integrity: a prospective comparative study. Fertil Steril 2008;89:375-379.PMID: 17509584.


2. Herbenick D, Reece M, Sanders SA, Dodge B, Ghassemi A, Fortenberry JD. Women's vibrator use in sexual partnerships: results from a nationally representative survey in the United States. J Sex Marital Ther 2010;36:49-65.PMID: 20063237.


3. Herbenick D, Reece M, Schick V, Sanders SA, Fortenberry JD. Women's use and perceptions of commercial lubricants: prevalence and characteristics in a nationally representative sample of American adults. J Sex Med 2014;11:642-652.PMID: 24521034.


4. Mowat A, Newton C, Boothroyd C, Demmers K, Fleming S. The effects of vaginal lubricants on sperm function: an in vitro analysis. J Assist Reprod Genet 2014;31:333-339.PMID: 24390681.



5. Frishman GN, Luciano AA, Maier DB. Evaluation of Astroglide, a new vaginal lubricant: effects of length of exposure and concentration on sperm motility. Fertil Steril 1992;58:630-632.PMID: 1521661.


6. Anderson L, Lewis SE, McClure N. The effects of coital lubricants on sperm motility in vitro. Hum Reprod 1998;13:3351-3356.PMID: 9886513.


7. Steiner AZ, Long DL, Tanner C, Herring AH. Effect of vaginal lubricants on natural fertility. Obstet Gynecol 2012;120:44-51.PMID: 22914390.



8. Settlage DS, Motoshima M, Tredway DR. Sperm transport from the external cervical os to the fallopian tubes in women: a time and quantitation study. Fertil Steril 1973;24:655-661.PMID: 4737661.


10. Goldenberg RL, White R. The effect of vaginal lubricants on sperm motility in vitro. Fertil Steril 1975;26:872-873.PMID: 1237417.


11. Homonnai T, Paz G, Sofer A, Yedwab GA, Kraicer PF. A direct effect of alpha-chlorohydrin on motility and metabolism of ejaculated human spermatozoa. Contraception 1975;12:579-588.PMID: 1192744.


12. Buch JG, Dikshit RK, Mansuri SM. Effect of certain volatile oils on ejaculated human spermatozoa. Indian J Med Res 1988;87:361-363.PMID: 3169889.

13. Anderson D. Genetic and reproductive toxicity of butadiene and isoprene. Chem Biol Interact 2001;135-136:65-80.PMID: 11397382.


-
METRICS

- Related articles in Clin Exp Reprod Med
-
Effects of a short abstinence period on sperm quality in oligozoospermic men2023 December;50(4)
Effects of Calcium and dbcAMP on Sperm Motility in Mouse1989 ;16(2)
Effect of pH and osmolarity on the sperm motility.1993 June;20(1)
Effects of infections with five sexually transmitted pathogens on sperm quality2017 December;44(4)
Effect of electromagnetic field exposure on the reproductive system2012 March;39(1)