Introduction
Uterine fibroids are the most common gynecological disorder in women of reproductive age. The prevalence of fibroids has been reported to vary from 20% to 50%. Fibroids are associated with subfertility in approximately 5% to 10% of cases [
1]. Previous studies have shown that most women affected by fibroids are fertile, although the fibroids may interfere with fertility secondarily to anatomical distortion and alterations of the uterine environment that can disrupt sperm movement [
2,
3]. Various factors, such as the size, location, and number of uterine fibroids, can alter the effect of fibroids on a woman's fertility status [
4]. Nonetheless, no definitive conclusion has been reached regarding the effect of uterine fibroids on
in vitro fertilization (IVF) outcomes, and this issue remains controversial. Many studies have showed that submucosal and intramural fibroids are associated with reduced implantation and pregnancy rates, particularly large uterine fibroids (e.g., >4 cm) [
5,
6], whereas other studies have failed to show such an association [
7,
8,
9,
10].
In addition to fibroids, some other factors are related to the success of IVF, such as uterine receptivity [
11,
12]. Doppler ultrasound examination is a noninvasive tool for examining uterine receptivity, which is thought to be a predictive factor for IVF outcomes [
13]. However, it is still controversial whether the uterine arteries reflect the actual blood flow of the endometrium. Moreover, several other recent studies have found that the role of subendometrial blood flow in predicting IVF outcomes is still subject to debate and requires further research [
14]. Most studies have used a long gonadotropin-releasing hormone (GnRH) agonist protocol in controlled ovarian stimulation (COS). However, the GnRH agonist protocol itself can affect fibroid growth by causing them to shrink, which could favorably influence IVF outcomes, thereby interfering with the ability of such studies to detect the effects of the fibroids themselves on IVF outcomes.
With this in mind, we carried out a retrospective study evaluating how uterine fibroids affected IVF results based on their size, number, and cavity-distorting effects, using a GnRH antagonist multiple-dose protocol. Additionally, we assessed changes in the resistance index (RI) and pulsatile index (PI) of the uterine artery and subendometrial artery, which can be altered by uterine fibroids.
Methods
This retrospective study was performed in a university-based infertility clinic at Asan Medical Center. The study population comprised 86 infertile patients who were treated with a GnRH antagonist multiple-dose protocol. The Institutional Review Board of Asan Medical Center, College of Medicine, University of Ulsan approved the study. The medical records of 86 patients with infertility who visited our clinic from January 2008 to March 2009 were reviewed. The treatment outcomes of 43 IVF cycles in 43 infertile patients with uterine fibroids were compared with those of 43 IVF cycles in 43 age-matched patients without fibroids. If patients underwent two or more cycles of IVF/intracytoplasmic sperm injection (ICSI) during the study period, the charts corresponding to the first IVF/ICSI cycle were reviewed and data from all other IVF/ICSI cycles were excluded from this analysis.
Patients with other uterine anomalies or a history of myomectomy were excluded from the study. Patients with current endocrine abnormalities such as diabetes mellitus or polycystic ovary syndrome, previous hospitalization due to severe ovarian hyperstimulation syndrome, a history of previous (within 12 months) or current abuse of alcohol or drugs, hyperprolactinemia, repeated implantation failure, or recurrent spontaneous abortion were also excluded from this study.
Uterine fibroids were detected by transvaginal sonography (TVS) (ProSound SSD-3500SV; Aloka, Tokyo, Japan) by a single experienced evaluator. The diagnosis of uterine fibroids was made at the patients' first visit. The uterus was visualized in both the sagittal and coronal planes to determine the absence or presence of fibroids and, if present, the type (intramural, subserosal, and submucosal) and location of the fibroids. If more than one fibroid was present, the mean value (length, height, and width) of the largest fibroid was selected for analysis. We defined cavity distortion to be absent if the endometrium-myometrium transition was clearly seen as a line in a TVS examination, without distortion of its contours by the presence of fibroids [
5]. Cavity distortion was defined by the presence of a fibroid encroaching on the uterine cavity line.
TVS color Doppler measurement of all patients was performed on the day of embryo transfer. The PI and RI of the uterine artery were calculated electronically when three or more similar waveforms of good quality were obtained from the ascending branch of the uterine artery on both sides of the cervix. The PI and RI of the subendometrial artery were assessed if subendometrial flow was detected within an area Ōēż10.0 mm from the apparent basal layer of the endometrium [
13,
15]. When a longitudinal view of the uterus was obtained, the Doppler cursor was positioned where subendometrial vessels with the strongest color signals were detected on the screen.
In all subjects, a GnRH antagonist multi-dose protocol was used for COS. Recombinant human follicle-stimulating hormone (rhFSH, Gonal-F; Merck Serono S.A., Geneva, Switzerland) at a dose of 150 to 225 IU/day was administered starting on the third day of the menstrual cycle. The rhFSH dose was adjusted according to the ovarian response every 3 to 4 days. When the mean diameter of the lead follicle reached 13 to 14 mm, the GnRH antagonist cetrorelix (Cetrotide, Merck Serono S.A.) was started at a dose of 0.25 mg/day and continued daily until an injection of 250 ┬Ąg of recombinant human chorionic gonadotropin (Ovidrel, Merck Serono S.A.) was administered subcutaneously to induce follicular maturation. When one or more follicles reached a mean diameter of Ōēź18 mm, transvaginal ultrasound-guided oocyte retrieval was performed. Subendometrial artery blood flow and uterine RI and PI were recorded on the day of embryo transfer. On the third day after oocyte retrieval, one to four embryos were transferred into the uterus. Luteal support was provided by administering 90 mg of vaginal progesterone gel (Crinone gel 8%; Merck Serono S.A.) once daily, starting on the day of oocyte retrieval. Pregnancy was confirmed by rising serum beta-human chorionic gonadotropin concentrations and by examination of the gestational sac using TVS.
All statistical analyses were performed using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). Values are presented as mean┬▒standard deviation. The Student's t-test, the chi-square test, or Fisher's exact test was used to compare the groups. The Student's t-test was used when a normal distribution was confirmed. The p-values <0.05 were considered to indicate statistical significance.
Results
Of the 86 patients, 44 (51.1%) achieved pregnancy after IVF treatment. In the fibroid group, the pregnancy rate was 48.8% (21 out of 43 patients), whereas the pregnancy rate in the control group was 53.4% (23 out of 43 patients). No significant differences were found in the characteristics of patients between the fibroid and control groups (
Table 1). The mean fibroid size was 31.6 mm. Moreover, the COS results were also similar between these two groups. No significant variation was found in the pregnancy rate or in the RI and PI indices of the subendometrial and uterine arteries.
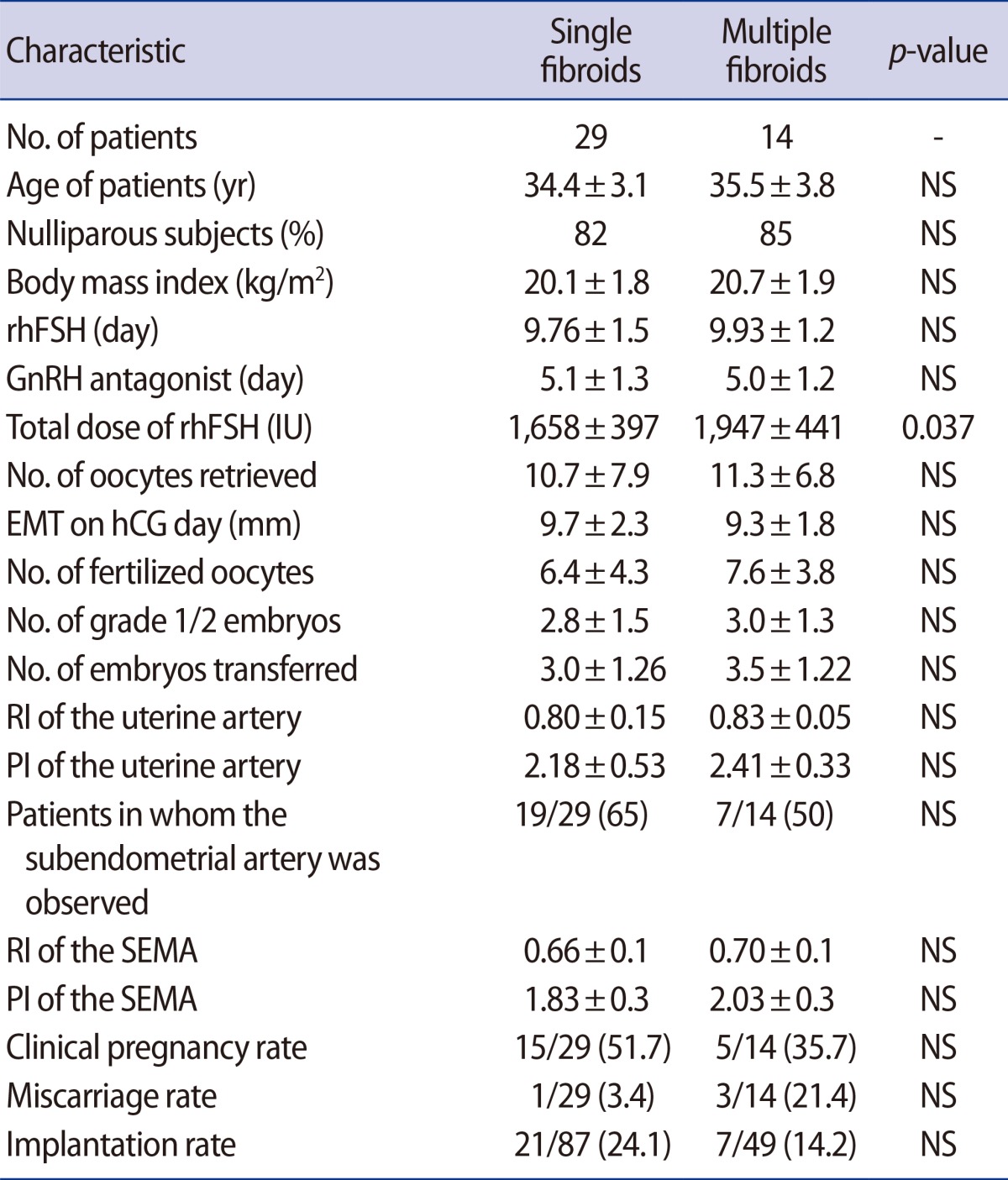
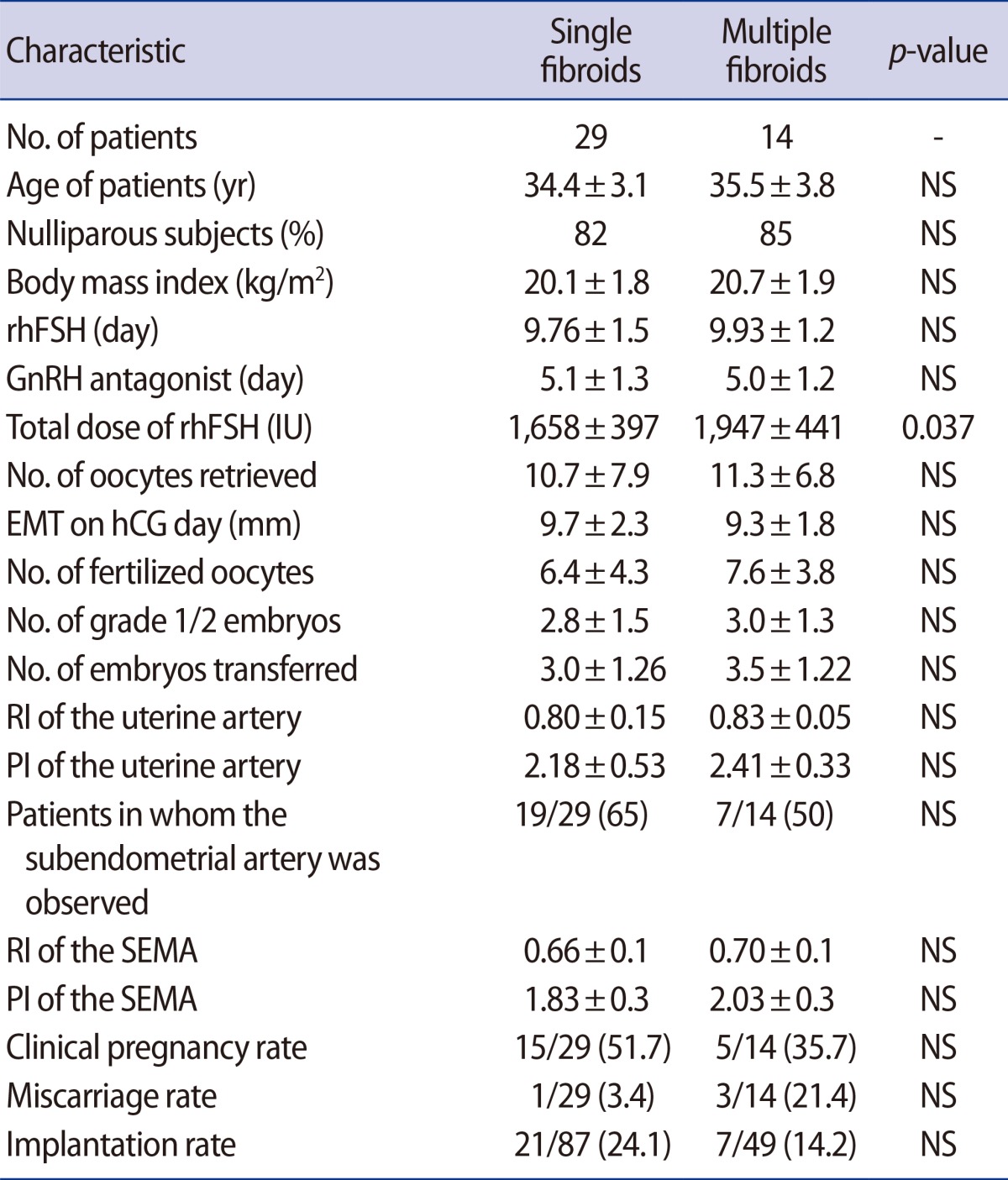
IVF outcomes and uterine hemodynamics were compared between women with single fibroids and multiple fibroids (
Table 2). The general characteristics of the patients in the single-fibroid and multiple-fibroid groups were found to be similar. Additionally, no significant differences were observed between these two groups regarding the duration of rhFSH and GnRH antagonist administration, but the total dose of rhFSH was higher in the multiple-fibroid group (
p=0.037). No significant differences were found between these groups in the pregnancy rate or in the RI and PI indices of the subendometrial and uterine arteries.
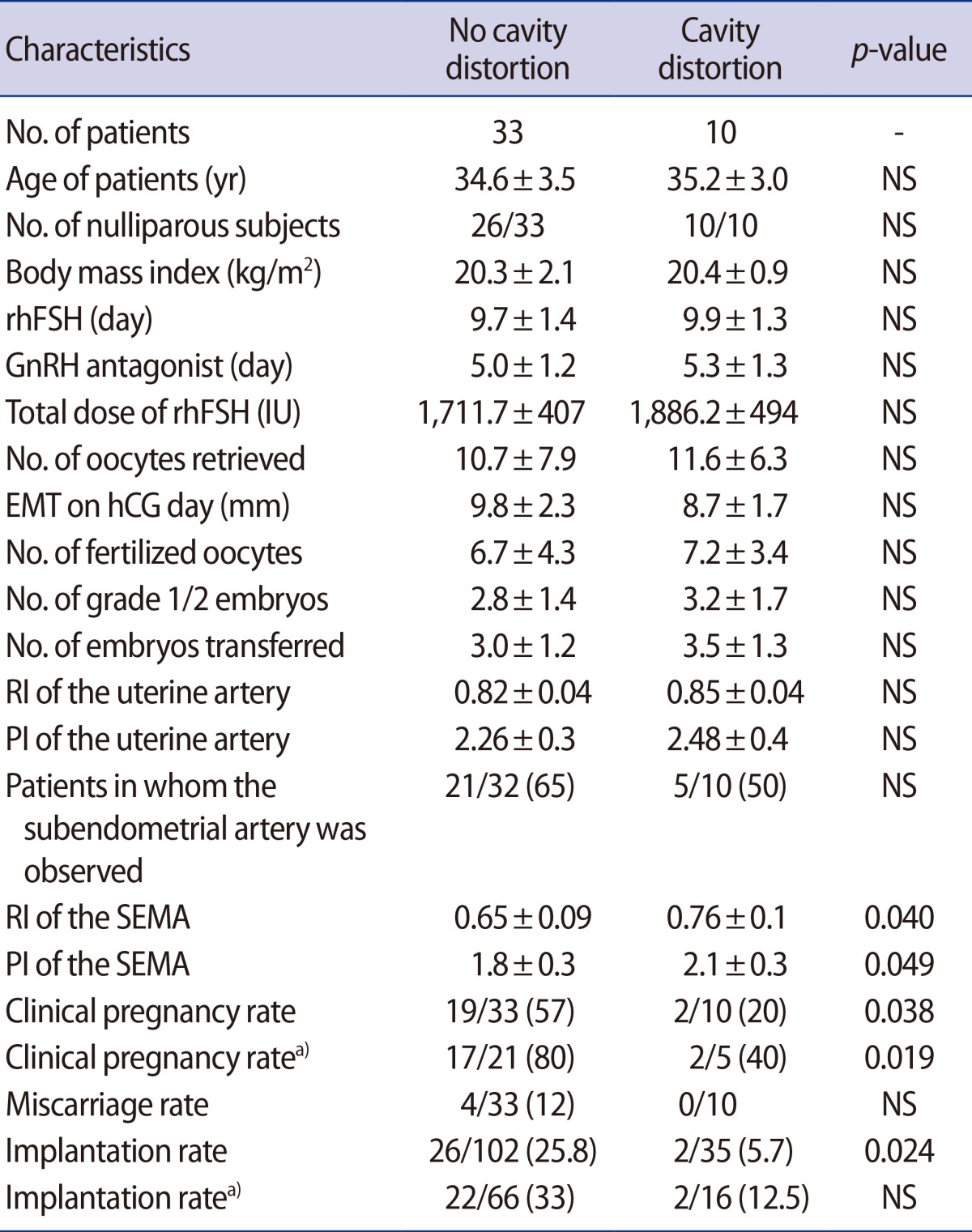
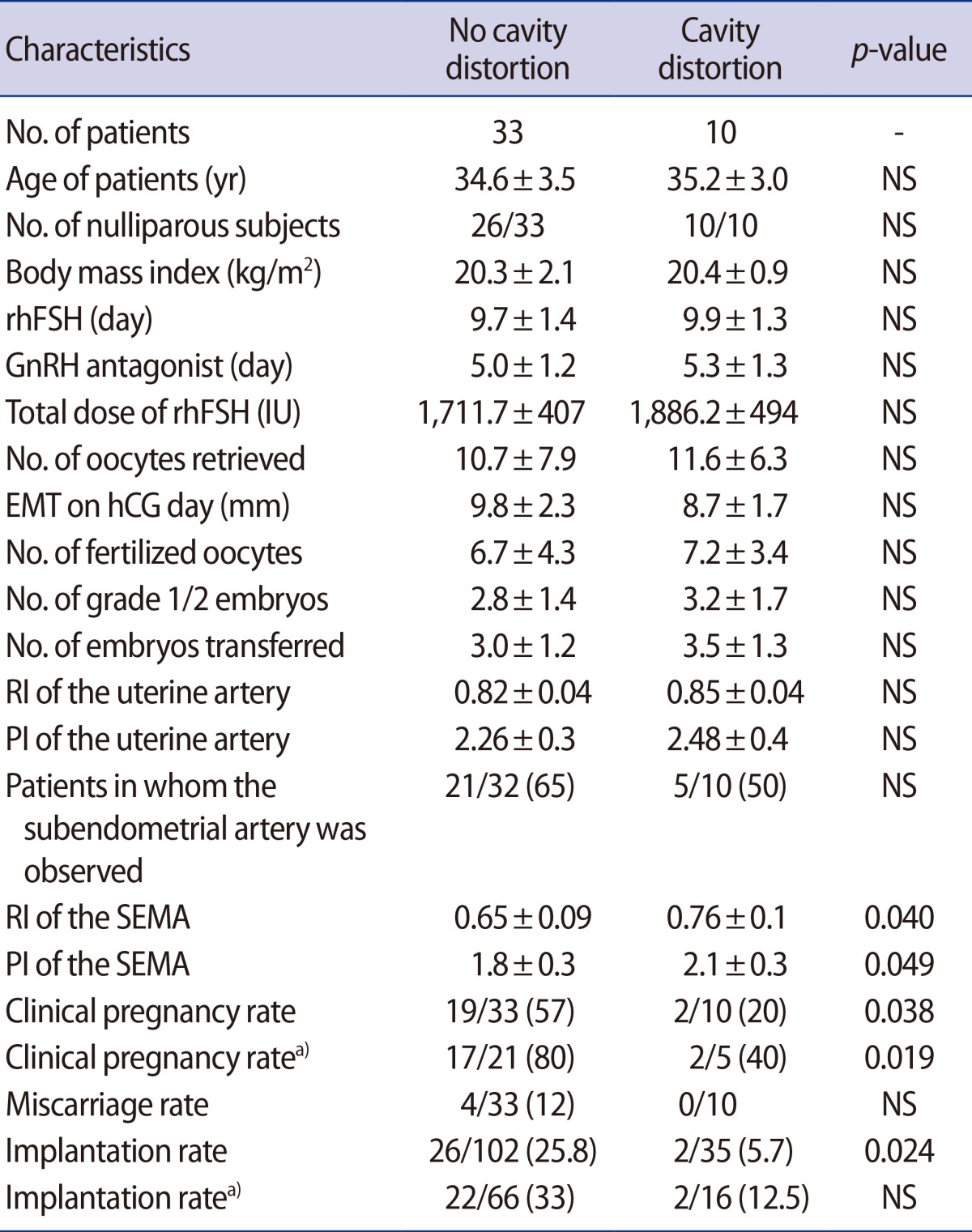
However, some significant differences were observed between women with fibroids who demonstrated cavity distortion and those who did not (
Table 3). The RI and PI indices of the subendometrial artery in the group without cavity distortion were significantly lower than in the group with cavity distortion. In addition, the clinical pregnancy rate was 57% in the group without cavity distortion and 20% in the group with cavity distortion (
p=0.038). The implantation rate was likewise higher in the group without cavity distortion than in the group with cavity distortion (25.8% vs. 5.7%,
p=0.024). A significant difference was also observed in the clinical pregnancy rate between these two groups among the subset of patients in whom the subendometrial artery was observed. Within this subset of patients, the clinical pregnancy rate was 80% (17/21) in the group without cavity distortion, compared to 40% (2/5) in the group with cavity distortion (
p=0.019).
Discussion
Previous studies have evaluated the effects of fibroids on the outcomes of IVF treatment using a GnRH agonist protocol for COS [
10]. However, the GnRH agonist protocol itself can impact fibroid growth, potentially causing size reductions that could favorably influence IVF outcomes and thereby confound the overall effects of fibroids on IVF results. Accordingly, instead of using a GnRH agonist protocol, we retrospectively selected patients who had used a GnRH antagonist for COS in order to avoid the favorable effects of the GnRH agonist protocol on fibroids. Additionally, we measured blood flow in the uterine and subendometrial arteries on the day of embryo transfer because previous researchers, including Zaidi et al. [
16], have suggested that the absence of subendometrial blood flow is associated with implantation failure, as well as to confirm the association between uterine artery blood flow and IVF outcomes [
17,
18,
19,
20]. Previous studies of the relationship between uterine hemodynamics and IVF outcomes only included normal uteri without fibroids [
17,
18,
19]. Unlike prior studies, our study included a group with fibroids, and we compared uterine hemodynamics on the day of embryo transfer between patients with or without uterine fibroids.
In the present study, no significant differences were found in IVF outcomes or in subendometrial and uterine artery blood flow depending on the presence of fibroids. Additionally, corresponding to previous studies [
7,
9], we found that small fibroids that did not distort the uterine cavity did not impair IVF outcomes. However, the effect of such fibroids on the IVF outcomes remains controversial. For example, Oliveira et al. [
5] noted that patients with intramural fibroids with a mean diameter >4.0 cm had lower pregnancy rates than patients with smaller intramural fibroids. Similarly, Hart et al. [
6] reported that intramural fibroids Ōēż5 cm had a negative impact on IVF results. Contrastingly, Ramzy et al. [
21] found that fibroids with a mean diameter <7 cm that did not encroach on the uterine cavity did not affect the outcomes of IVF or ICSI. Analogously, Check et al. [
10] reported that small (<5 cm) intramural fibroids that did not compress the uterine cavity had no effect on IVF outcomes. Similarly to previous studies, our study included fibroids with a mean size of 31.6 mm and found that they had no impact on IVF results, although we did observe adverse IVF treatment outcomes when cavity distortion due to fibroids was present.
No significant differences in IVF outcomes or in uterine artery and subendometrial artery blood flow were observed between the single- and multiple-fibroid groups. The only significant difference observed was in the total dose of recombinant FSH used in COS. The cause of this difference is not certain. It could have reflected bias present in our study. Alternately, some fibroids in the multiple-fibroid group could have affected the ovarian arterial blood flow, disturbing the growth of follicles during COS. The anatomical location of the fibroid is expected to be highly relevant in terms of its influence on fertility status and pregnancy maintenance [
22]. In order to test this assumption, subsequent studies should subdivide patients by fibroid location and investigate ovarian arterial blood flow during COS.
Similarly to earlier studies [
17,
18] that did not include fibroids, we found no association between uterine artery blood flow and IVF outcomes, regardless of the presence of uterine fibroids. Wang et al. [
18] reported that the PI index and RI index of the endometrial spiral arteries were much lower in patients who became pregnant than in patients who did not, in a study exploring the utility of Doppler imaging for predicting pregnancy outcomes in IVF cycles. Similarly, in our study, the group without cavity distortion had lower PI and RI indices of the subendometrial artery and had higher pregnancy rates than the group with cavity distortion.
The results of the present study are of note because we used a GnRH antagonist protocol instead of a GnRH agonist protocol for COS in order to avoid the favorable effects of GnRH agonists on fibroids. Moreover, we studied uterine hemodynamics in the presence of uterine fibroids. However, our small sample size and retrospective study design are limitations of this study. Additionally, we also had inadequate information regarding the precise location of the fibroids. A prospective randomized trial including the precise localization of uterine fibroids is necessary to overcome the weaknesses of our current study.
In conclusion, if no distortion of the uterine cavity is present, neither IVF outcomes nor blood flow in the uterine and subendometrial arteries on the day of embryo transfer are influenced by the presence of fibroids. However, uterine fibroids that distort the uterine cavity not only impair subendometrial artery blood flow, but also negatively affect the rates of implantation and clinical pregnancy in patients undergoing IVF.
Table┬Ā1
IVF parameters and pregnancy outcomes depending on the presence of fibroids

Table┬Ā2
IVF parameters and pregnancy outcomes according to the presence of single or multiple fibroids
Table┬Ā3
IVF parameters and pregnancy outcomes depending on whether uterine fibroids caused distortion of the endometrial cavity